The latest updates and information Mississippi Medicaid providers need to know is posted in Late Breaking News
1/29/2026
Provider Disenrollment FAQs
Disenrollment Due to Claims Inactivity
In accordance with provider directory requirements at 42 U.S. Code 1396a, any enrolled Medicaid provider not appearing on a submitted claim within the past 12 months will be disenrolled, effective February 1, 2026. For further details, please see the Mississippi Administrative Code, Title 23, Part 200, Rule 4.2 (A) 17.
My provider enrollment was just approved, what can I do to ensure I am not disenrolled for claim inactivity?
Newly enrolled providers will have up to one (1) year from the effective date of enrollment to appear on a submitted claim before being subject to disenrollment. To prevent disenrollment, providers should submit claims as services are rendered to Medicaid members.
If I have multiple service location enrollments will all locations be disenrolled if only one location does not have any claims activity?
No, only the servicing locations with no claim activity will be disenrolled.
How will I be notified if I am disenrolled?
Each disenrolled provider will receive a notification letter informing them of the disenrollment by mail sent to the mail to address on file with DOM. As noted in the December 30, 2024, Late Breaking News article, the notification will also be available for viewing in the provider portal.
What can I do if I am disenrolled?
Providers disenrolled due to inactivity may submit an application to re-enroll in the Medicaid program at any time. For more information, call the Provider and Beneficiary Services Call Center at 1-800-884-3222 or your designated field representative: https://medicaid.ms.gov/wp-content/uploads/2025/09/Q3-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County_v1.0.pdf.
1/23/2026
State of Emergency & Medicaid Pharmacy Billing Guidance
The Governor has declared a State of Emergency in advance of severe winter weather expected to impact Mississippi beginning Friday, Jan. 23, 2026. The declaration will remain in effect through at least Jan. 27 and allows the state to mobilize resources and support response efforts in affected counties. During the State of Emergency, pharmacies should follow emergency billing procedures, including the use of applicable emergency overrides, to ensure continuity of care for members.
Pharmacy POS Billing During Officially Declared Emergencies
During an officially declared state of emergency, pharmacy providers may override service limits by submitting POS claims with NCPDP Field 420-DK = “13 – Payer Recognized Emergency.” This override applies to:
- • 2 Brand / 6 Prescription limit
• Early refill edits
These fields will be opened for the duration of the declared emergency. Providers should use professional judgment when dispensing medications. The Division of Medicaid may conduct post-event audits to ensure appropriate use. Providers and members outside of affected areas must maintain documentation supporting early or excess fills. Claims may be subject to recoupment if documentation is insufficient.
1/22/2026
New Taxonomy Available for MSCAN and FFS
Effective immediately, taxonomy code 261QU0200X (Clinic or Center – Urgent Care) is now available for MississippiCAN (MSCAN) and Fee-for-Service (FFS) providers. Previously, this taxonomy code was limited to CHIP only.
Providers may submit taxonomy change requests by including the 9-digit Medicaid ID and the requested taxonomy code using one of the following secure submission methods:
Online – MESA Provider Portal (Preferred Method)
Access the Secure Correspondence link on the MESA Provider Portal:
https://medicaid.ms.gov/mesa-portal-for-providers
For requests involving multiple Medicaid IDs, please attach a spreadsheet listing each update as a separate row.
Fax
Fax Number: (866) 644-6148
Attention: Provider Enrollment
Mailing Address:
Provider Enrollment
P.O. Box 23078
Jackson, MS 39225
The requested taxonomy code must match the taxonomy reported in the NPPES NPI Registry to ensure accuracy and compliance.
If you have any questions or need further assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or refer to the Provider Field Representative list on Medicaid’s website, which includes email addresses and phone numbers for each representative. This list is available at https://medicaid.ms.gov/wp-content/uploads/2025/09/Q3-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County_v1.0.pdf.
1/21/2026
Reminder about claims suspension:
11/20/2025
Claims Suspension Due to Missed Deadline
Effective February 1, 2026, the Mississippi Division of Medicaid (DOM) will begin suspending submitted claims for providers that fail to submit their Revalidation or Recredentialing application by the due date indicated on the notice, which is 60 days after the Revalidation or Recredentialing Notice is mailed. Additionally, providers are reminded of the Application Submission Due Date column in the Six-Month Recredentialing Due List and the Six-Month Revalidation Due List that is posted on the DOM website, which is updated twice a month. DOM encourages timely submission of Revalidation and Recredentialing applications to avoid unnecessary disruption of claims processing for the provider.
Failure to submit the revalidation or recredentialing application by the Application Submission Due Date will result in Fee-for-Service claim suspension until the application is submitted.
Providers who submit their Revalidation or Recredentialing applications before the due date will avoid claim suspension; however, those who submit after the due date may encounter delays in claims processing and will receive the following Explanation of Benefits (EOB) on their submitted claims:
- • 2080 – BILLING PROVIDER ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2081 – HEADER RENDERING PROVIDER ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2082 – DETAIL RENDERING PROVIDER ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2083 – HEADER ATTENDING PROVIDER ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2086 – HEADER OPERATING PROVIDER-1 ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2087 – HEADER OTHER/OPERATING PROVIDER-2 ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2088 – DETAIL OPERATING PROVIDER-1 ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2089 – DETAIL OTHER/OPERATING PROVIDER-2 ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
Claims will be released from suspension once the revalidation or recredentialing application is submitted by the provider.
Providers should ensure their mailing address is up to date to receive notifications promptly.
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or contact your designated Provider Field Representative.
12/18/2025
Provider Enrollment Application Fee Increase for 2026
Effective January 1, 2026, the enrollment application fee for institutional providers will increase from $730 to $750 for the 2026 calendar year. Additional details are available in the official federal announcement (Federal Register).
The application fee applies to the following provider transactions within Medicaid (Fee-for-Service), MSCAN and/or the Children’s Health Insurance Program (CHIP):
• Initial enrollment, reactivation, revalidation, or reenrollment
• Addition of new owners (Change of Ownership)
• Addition of a new Medicaid practice location
Note: Routine updates to provider information—such as changes to phone numbers, bank account details, billing addresses, or provider names—do not require payment of the application fee.
To review the list of taxonomies subject to the application fee, please review the DOM website.
Providers submitting their application fee should make their check payable to the Mississippi Division of Medicaid, noting the application tracking number (ATN) on the check and mail it to:
Gainwell Technologies
P.O. Box 6014
Ridgeland, MS 39158.
Providers who have already paid the application fee to Medicare or another state’s Medicaid or CHIP program have fulfilled the requirement and do not need to pay the fee again to Mississippi Medicaid.
For more information, call the Provider and Beneficiary Services Call Center at 1-800-884-3222 or your designated field representative.
12/18/2025
Portal Account Inactivity Deactivation and Reactivation for Providers/Members/Delegates/Trading Partners
In accordance with CMS requirements, MESA Portal accounts for all users (providers, members, delegates and trading partners) will be deactivated after 15 months of inactivity starting December 29, 2025. To retain access to the MESA Web Portal, users are encouraged to log in periodically. A note about Delegate Accounts: Delegates will retain access to the provider’s accounts if the provider is active in MESA or the provider has been inactive in MESA for one year or less.
How can I prevent my account from being deactivated?
To maintain active status, log in to your MESA Web Portal account at least once every fifteen (15) months.
What will occur when my account is deactivated?
Your Portal account will be placed in a disabled status, and an email notification will be sent to the email address on file. The email will have directions for reactivating the account as follows:
If you wish to reactivate your account, please follow the reactivation instructions provided below:
- Go to the MESA Portal Home Page.
- Enter your User ID and then click the Sign In button.
- An email will then be sent with further instructions and a secure link to complete the reactivation process.
How do I reactivate my MESA Portal Account?
To reactivate, navigate to the MESA Portal, enter your user id and select Log In. If your account has been disabled, you will be redirected to the Home Page with the following message: “Your MESA Web Portal account has been disabled due to inactivity. An email has been sent to the email address on file with instructions to reactivate your MESA Web Portal account.”
The email will contain a secure time-limited reactivation token and a link to initiate the reactivation process. The reactivation token will be valid for 3 days from the time of generation.
Upon clicking the link in the email, the user will be redirected to a Web Portal page where they can enter the token (received in the email) and click the reactivate button to complete the process.
What if my token has expired?
If the token is expired or entered incorrectly, the user will be displayed with a message “Token is invalid or expired. Please try entering token again or regenerate a new token using the “Regenerate Token” button below.
When a user clicks on the ‘Regenerate Token’ button, the system will generate a new token and send to the user’s email address. System will also display a message to the user “An email has been sent to the email address on file with instructions to reactivate your MESA Web Portal account.”
Once the account is successfully reactivated, the user will be redirected to the Web Portal Home Page to restart the login process.
Support and Resources
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative.
The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/09/Q3-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County_v1.0.pdf.
12/11/2025
HCBS Rate Updates effective 1/1/2026
For dates of service on or after January 1, 2026, the rates for services on the 1915(c) and 1915(i) home and community-based services programs have been increased and will be paid in accordance with the updated fee schedule below. The appropriate taxonomy, procedure code and modifier combinations outlined in the table must be utilized for billing these services.
Providers of services requiring electronic visit verification (EVV) will need to manually update their Billing Rate for each in the EVV system on Thursday, January 1, 2026, prior to submitting claims. Instructions on how to complete those updates can be found in the HHAX Knowledge Base at https://knowledge.hhaexchange.com/provider/Content/Documentation/Admin/Admin-C-Rate-Management-S.htm?Highlight=rates.
12/10/2025
Maintenance set for Pharmacy POS firewall
Gainwell Technologies, the Fiscal Agent for the Mississippi Division of Medicaid, will conduct server maintenance affecting the routing of pharmacy transactions for CoverMyMeds (CMM, formerly RelayHealth), Change Healthcare (CHC), and RedSail Pharmacy POS, as outlined below:
Date: December 11, 2025 (details as follows):
o 12:00 a.m. Central – Maintenance Activity start time.
o 1:00 a.m. Central – Maintenance complete and POS transactions submissions can resume.
Providers are encouraged to not submit claims during this window of time. Should you need additional information, please contact the Gainwell pharmacy help desk at (833) 660 2402.
12/2/2025
System experiencing periodic timeouts for POS transactions/EDI real-time transactions
The Mississippi Division of Medicaid’s claims system has been experiencing periodic high timeouts for POS and other EDI real-time transactions. There were 328 timeouts yesterday and at least 179 today at different times of the day. The service is up and responding at this time, but we are closely monitoring. Our team is working to determine what is causing these periodic timeouts since these timeouts are happening during EDI transformations.
We will post updates as they become available.
12/2/2025 – RESCINDED – DOM has elected to delay moving forward with the planned revisions to the Hospital-Based Clinic policy.
Attention: Hospitals and Hospital-Based Clinics
Effective January 1, 2026, the Mississippi Division of Medicaid (DOM) will no longer recognize Hospital-Based Clinic billing. DOM will not reimburse the facility fee for evaluation and management (E&M) codes on the institutional claims (UB-04/837I transactions) for hospital-based clinic services.
E&M codes (with the exception of Emergency Room E&Ms) billed on an institutional claim will be denied when billed by the facility for hospital-based clinic services. When beneficiaries are referred to or sent from the clinic to the hospital to receive outpatient services (e.g. lab or imaging), providers will continue to bill these services on the institutional claim.
Hospital-based clinics that are within or outside your hospital walls will be considered independent clinics. These services are provided by an individual physician or non-physician practitioner in the clinic and must be billed on a CMS 1500 with place of service 11.
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/09/Q3-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County_v1.0.pdf.
11/26/2025
Update to Medicaid Eligibility Search Timeframe
Effective immediately, the Medicaid eligibility search window has been expanded from 3 years to 5 years.
This change applies across all eligibility inquiry methods, including:
· Provider Portal
· EDI (Electronic Data Interchange)
· AVRS (Automated Voice Response System)
Regardless of the platform used, all Medicaid eligibility searches will now return up to five years of historical data. This update is intended to improve access to comprehensive eligibility information and support more accurate verification and billing processes.
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or contact your designated Provider Field Representative.
11/25/2025
Electronic Visit Verification (EVV) Compliance Updates
Mississippi Medicaid Administrative Code Part 200 updates requiring EVV compliance will be effective 12/1/2025. The regulation, including a list of services for which EVV compliance is required, is available at https://www.sos.ms.gov/adminsearch/ACProposed/00028324b.pdf.
For Dates of Service 1/1/2026 forward, DOM will also be implementing a new edit in MESA to suspend any fee-for-service claims for EVV mandated services that do not originate from the HHAeXchange system. This step is necessary to ensure that DOM is compliant with federal requirements to require the capture of EVV data as defined in the 21st Century Cures Act prior to payment of claims. DOM staff will be reviewing those suspended claims to determine if providers have technical issues preventing the proper submission of claims from the state’s aggregator. If there is no technical issue, those claims will be denied and providers will be redirected to submit them via the aggregator. Starting 1/1/2026, providers with ongoing technical issues can submit a request to temporarily continue billing directly in MESA at the below link. DOM will review each case and authorize exceptions where needed to allow time to resolve technical issues while preventing delays in reimbursement.
https://app.smartsheet.com/b/form/755b455f96164333998cb78939b9558e.
For private duty nursing and home health services rendered to beneficiaries enrolled in MSCAN and MSCHIP, providers will be required to submit EVV data to the state’s aggregator with HHAeXchange but continue to submit claims directly to each of the managed care organizations. Magnolia, Molina, and TrueCare will be implementing similar edits on or after 1/1/2026 that require EVV data be submitted to them via the HHAeXchange aggregator prior to the payment of claims.
More information on the EVV implementation along with training resources are available at https://www.hhaexchange.com/info-hub/mississippi. Any additional questions regarding EVV compliance requirements can be emailed to DOM at evv@medicaid.ms.gov.
11/20/2025
Claims Suspension Due to Missed Deadline
Effective February 1, 2026, the Mississippi Division of Medicaid (DOM) will begin suspending submitted claims for providers that fail to submit their Revalidation or Recredentialing application by the due date indicated on the notice, which is 60 days after the Revalidation or Recredentialing Notice is mailed. Additionally, providers are reminded of the Application Submission Due Date column in the Six-Month Recredentialing Due List and the Six-Month Revalidation Due List that is posted on the DOM website, which is updated twice a month. DOM encourages timely submission of Revalidation and Recredentialing applications to avoid unnecessary disruption of claims processing for the provider.
Failure to submit the revalidation or recredentialing application by the Application Submission Due Date will result in Fee-for-Service claim suspension until the application is submitted.
Providers who submit their Revalidation or Recredentialing applications before the due date will avoid claim suspension; however, those who submit after the due date may encounter delays in claims processing and will receive the following Explanation of Benefits (EOB) on their submitted claims:
- • 2080 – BILLING PROVIDER ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2081 – HEADER RENDERING PROVIDER ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2082 – DETAIL RENDERING PROVIDER ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2083 – HEADER ATTENDING PROVIDER ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2086 – HEADER OPERATING PROVIDER-1 ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2087 – HEADER OTHER/OPERATING PROVIDER-2 ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2088 – DETAIL OPERATING PROVIDER-1 ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
• 2089 – DETAIL OTHER/OPERATING PROVIDER-2 ON SUSPENSION DUE TO MISSED APPLICATION REVALIDATION OR RECREDENTIALING
Claims will be released from suspension once the revalidation or recredentialing application is submitted by the provider.
Providers should ensure their mailing address is up to date to receive notifications promptly.
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or contact your designated Provider Field Representative.
11/17/2025
View Job Aid to Adjust or Void a Claim Via the Provider Portal
The Mississippi Division of Medicaid (DOM) has published a new job aid: “Adjust or Void a Claim Via the Provider Portal.” This resource provides step-by-step guidance for providers on how to adjust or void previously paid claims.
Key Requirements for Adjusting or Voiding a Claim:
- • Only paid claims can be adjusted or voided. Denied claims cannot be adjusted; a new claim must be submitted.
• Claim Status must be ‘Finalized Payment’ before initiating an adjustment or void.
• Voiding a claim removes the original claim and payment from history and may trigger Accounts Receivable (AR) for recoupment.
• Adjusting a claim allows corrections to billing codes, service dates, units, modifiers, place of service, referring provider ID, diagnosis codes, or charges.
• Attachments from the original claim do not auto-populate; providers must upload required documents again.
• Adjustments may result in additional payment or AR setup for recoupment.
• Use Print Preview before confirming submission to ensure accuracy.
Access the full job aid here: https://medicaid.ms.gov/wp-content/uploads/2025/11/PRP-101-Adjust-or-Void-a-Claim-Via-Provider-Portal-v0.2.pdf
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/09/Q3-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County_v1.0.pdf
10/27/2025
Request for Information Email Inbox to be Phased Out
As part of our ongoing efforts to streamline requests and improve efficiency at the Mississippi Division of Medicaid, the Request for Information email inbox (RFI@medicaid.ms.gov) is being phased out and is no longer actively monitored. Please see below for updated instructions on how to submit your request through the appropriate channel to ensure an accurate and timely response.
Helpful Information
For guidance and support for your specific needs, please contact your Provider Field Representative for assistance. You can access the list of Provider Field Representatives, which includes the email address and phone number for each representative at the following link: Provider Field Representatives Map and Contact List.
You will find detailed contact information for external information requests on the Contact page of the Mississippi Division of Medicaid website. If you are looking for a specific form, be sure to check out our updated list of forms on the Forms page of our website.
Be sure to note the Provider drop down for quick access to common contact information.
Common Forms/Inquiries
• Managed Care Provider Inquiry and Issue Form
• Eligibility Data Match Requests (New)
• Claim or Lein Requests (New)
We continue to appreciate your commitment to providing quality care to Medicaid beneficiaries and encourage you to utilize these resources for further assistance. For additional support, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222.
10/13/2025
Nursing home payment methodology to transition from RUG-IV to Patient-Driven Payment Model (PDPM)
Due to the Centers for Medicare and Medicaid Services (CMS) October 1, 2019 decision to replace the RUG-IV assessment, the Mississippi Division of Medicaid (DOM) will no longer use RUG-IV for its case mix reimbursement payment methodology. Effective January 1, 2026, the nursing home payment methodology will transition to the Patient-Driven Payment Model (PDPM).
Training sessions will be held to help providers prepare for this transition. To learn more and to register for training sessions, click on the links below:
• Transition from RUG-IV to PDPM Memo
• Mississippi Nursing Facility PDPM Reimbursement Training
10/6/2025
Important Provider Affiliation Updates and Guidance to Prevent or Resolve Denials with EOB/Error Code 1085
Facilities and other organizational providers can now affiliate individual providers to their organizational provider enrollment. This affiliation addresses some prior authorization (PA) issues that were impacting the Managed Care Organizations (MCOs). As organizational providers begin affiliating individual rendering providers, certain fields on professional claims (CMS-1500) may require modification to ensure accurate claim processing.
Certain provider types are not required to include a separate rendering provider on the claim form and must use the Billing Provider information in the Rendering Provider fields. Example: when the billing provider is a facility and the rendering provider is not eligible for enrollment with Mississippi Medicaid.
Organizational providers who receive Explanation of Benefits (EOB) Error Code 1085, which indicates “Provider is a facility or group provider. A rendering provider is required,” on professional claims must verify that valid rendering provider information is included in the appropriate claim field.
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/05/Q2-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County_v2.0.pdf.
9/24/2025
Incontinence Garment Prior Authorizations
Beginning July 1, 2025, a configuration issue affected the processing of prior authorizations for incontinence garments — specifically diapers, pull-ups, and blue pads. These items were not properly accounted for, resulting in premature exhaustion of authorized amounts.
The Division of Medicaid (DOM) has identified the root cause and implemented a fix to prevent further occurrences. DOM is in the process of identifying impacted PAs and Claims and will reprocess Claims submitted with dates of service (DOS) on or after 07/01/2025 thru 09/05/2025.
9/23/2025
Xifaxan and Trulance Coverage Update
Effective October 1, 2025, Bausch Health Companies (including Bausch + Lomb and Salix Pharmaceuticals) will withdraw from the Medicaid Drug Rebate Program (MDRP). Under federal requirements, the Division of Medicaid (DOM) is not obligated to cover medications from manufacturers that do not participate in the MDRP.
As a result, Xifaxan and Trulance will no longer be covered by Mississippi Medicaid beginning October 1, 2025.
To support affected patients, Bausch Health has established a patient assistance program specifically for Medicaid members. Program details and application materials are available at the Bausch Health Patient Assistance Program.
Important: At this web address, there are two application links. For Mississippi Medicaid members, please be sure to use the “Application for Medicaid-only Patients” link.
9/22/2025
Important Reminder: Timely Filing Review Requests
The Division of Medicaid (DOM) reminds providers that all timely filing review requests submitted to DOM online, by mail, or by facsimile must include a formal letter.
Your letter should:
• Describe the issues relevant to the timely filing denial.
• Provide justification for consideration during the review.
In addition, providers must submit all supporting documentation that substantiates the request. Please note that failure to provide all required documentation may result in delays to your review.
Administrative Code References
Providers should review the following sections of the Administrative Code for guidance:
• Part 200, Rule 1.6: Timely Filing
• Part 200, Rule 1.7: Timely Processing of Claims
• Part 200, Rule 1.8: Administrative Review for Claims
• Part 300, Chapter 4: Claim Denials for Policy Regarding Administrative Reviews
The full Administrative Code can be accessed here: Mississippi Medicaid Administrative Code.
Please note that specific documentation requirements are detailed in Part 200, Rule 1.8(B).
Next Steps for Providers
When submitting a timely filing review request:
• Include a formal letter with your request.
• Clearly explain the issues related to the timely filing denial.
• Provide justification for DOM to consider.
• Attach all supporting documentation.
• Reference the applicable Administrative Code rules to ensure compliance.
9/18/2025
MS Medicaid Crossover Cover Sheet – Effective October 1, 2025
Effective October 1, 2025, Mississippi Medicaid will require use of the MS Medicaid Crossover Cover Sheet for all crossover claims submitted via paper. Paper claims submitted without the new form and the Explanation of Medicare Benefits (EOMB), or completed incorrectly will be returned unprocessed.
Proper completion of this form allows Gainwell to accurately scan and key your paper claim with the correct claim type and filing indicators—ensuring faster and more accurate processing. The updated form and instructions are available under the “Provider Forms” section of DOM’s website: https://medicaid.ms.gov/resources/forms/.
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at Q3-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County_v1.0.pdf.
9/9/2025
Reminder to PPEC Providers
Effective June 2021, the Mississippi Division of Medicaid (DOM) made changes to the way transportation services were billed by Prescribed Pediatric Extended Care (PPEC) providers. As a result, for dates of services on or after July 1, 2021, PPEC centers that provide transportation are required to submit monthly trip logs to DOM.
Trip logs should be submitted to the Office of Health-Related Programs and Benefits (formerly the Office of Medical Services) no later than the tenth (10th) business day of the month following the month that the services were rendered. (Example: The trip log for service month of June 2025 must be submitted to DOM no later than the close of business (COB) on July 14. 2025.) Trip logs should be emailed to the Office of Health-Related Programs and Benefits at HRPB@medicaid.ms.gov or faxed to 601-359-6147. Failure to submit monthly trip logs may result in claim payments being held.
If you have any questions, please contact the Office of Health-Related Programs and Benefits at 601-359-6150 or HRPB@medicaid.ms.gov.
9/9/2025
Rendering/Facility Provider Usage Change
The Mississippi Division of Medicaid (DOM) will reprocess claims where the claim was not submitted with a rendering provider ID, or the rendering provider ID was invalid. The claims process used the following NPI matching for the NPI Crosswalk of Rendering providers.
- One to One match using the NPI to the Billing Provider Group. If no match was found, then…
- One to One match using the Providers listed in the Billing provider group and the Rendering Taxonomy. If no match, then…
- One to One match using the Providers listed in the Billing provider group, Rendering Taxonomy and the Zip+4 from the Facility Provider, if Present on the claim. If No Facility Provider is submitted on the claim, then use the Zip+4 from the Billing Provider submitted Address. If no match, then…
- The claim/detail(s) denied with provider billing edits.
Providers impacted by this Mass Adjustment (MA) should submit a corrected claim for payment. In the event that the corrected claim(s) deny for timely filing, providers are reminded that in accordance with Part 200, Rule 1.8(A)(2), providers may request an Administrative Review regarding claims within ninety (90) calendar days of the denial of a claim, when the Division of Medicaid adjusts claims after timely filing and timely processing deadlines have expired. Requests for an Administrative Review must include documentation that explains the facts that support the provider’s position as to how the denied claim meets one (1) or more of the requirements in Miss. Admin. Code, Title 23, Part 200, Rule 1.8.A. and the reasons the provider believes he/she complied with Medicaid regulations, and other documentation as required or requested by DOM.
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/04/Q2-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County.pdf.
9/8/2025
Updated Sterilization Consent Form
The Office of Population Affairs has released the updated sterilization form with a new expiration date of 7/31/2028. All sterilizations require a valid consent form. Providers are responsible for using the most current form published on the date the consent is obtained. Effective September 15, 2025, the Division of Medicaid (DOM) will no longer accept sterilization consent forms with the expiration date of July 1, 2025. The current sterilization consent form is available in English and Spanish under the “Provider Forms” section of DOM’s website: https://medicaid.ms.gov/resources/forms/.
Additional information regarding policy and procedures for sterilizations can be found in the Mississippi Administrative Code Title 23 at Administrative Code Part 202 Chapter 5 Rule 5.3.
8/8/2025
Pharmacy POS firewall to be upgraded
We would like to inform you that Gainwell Technologies, Fiscal Agent for the Mississippi Division of Medicaid, is upgrading the firewall for routing pharmacy transactions for Cover My Meds (CMM, formerly Relay Health), Change Healthcare (CHC), and RedSail Pharmacy POS as follows:
- • Date: August 10, 2025 (details as follows):
- o 12:00 a.m. Central – Upgrade Activity start time.
- o 2:00 a.m. Central – Upgrade complete and POS transactions submissions can resume.
Providers are encouraged to not submit claims during this window of time. Should you need additional information, please contact the Gainwell pharmacy help desk at 1-833-660-2402.
8/6/2025
Request for Information Email Inbox to be Phased Out
As part of our ongoing efforts to streamline requests and improve efficiency at the Mississippi Division of Medicaid (DOM), the commonly used Request for Information email inbox (RFI@medicaid.ms.gov) is being phased out and is no longer actively monitored. Please see below for updated instructions on how to submit your request through the appropriate channel to ensure an accurate and timely response.
Questions and Information Requests
For most provider questions the first place to start is to contact your Provider Field Representative for assistance. You can access the list of Provider Field Representatives, which includes the email address and phone number for each representative, at the following link: Provider Field Representatives Map and Contact List.
For different types of information requests, you can find a number of helpful resources on DOM’s Contact webpage, including instructions on how to submit a request for public records.
If you are looking for a specific form, be sure to check out our updated list of forms on the Forms page of our website.
Be sure to note the Provider drop down for quick access to common contact information.
Common Forms/Inquiries Recently Updated
- Managed Care Provider Inquiry and Issue Form
- Eligibility Data Match Requests
- Subrogation Form (Claim or Lein Requests)
We value your partnership and your commitment to providing quality care to Medicaid beneficiaries, and we encourage you to use these resources to meet the needs of all our stakeholders.
8/1/2025
Pharmacy POS processing server upgrade
We would like to inform you that the current processing server for pharmacy transactions for Cover My Meds (CMM, formerly Relay Health), Change Healthcare (CHC), and RedSail Pharmacy POS transaction processing is going to be upgraded as follows:
• Date: August 3, 2025 (details as follows):
o 6:00 AM Central – Processing server upgrade Activity start time.
o 10:00 AM Central- Upgrade complete and POS transactions can be submitted.
Providers are encouraged to not submit claims during this window of time. Should you need additional information, please contact the Gainwell pharmacy help desk at 1-833-660-2402.
8/1/2025
Pharmacy Point-of-Sale Drugs: Prior Authorization Requirements
Effective October 1, 2025, the Mississippi Division of Medicaid (DOM) will require prior authorization (PA) of the following pharmacy point-of-sale (POS) drugs:
Drug Name, Strength, and Formulation
ABELCET 100 mg/20 mL vial
AMBISOME 50 mg vial
amphotericin B 50 mg vial
amphotericin B liposome 50 mg vial
AVYCAZ 2.5 g vial
CANCIDAS IV 50 mg vial
CANCIDAS IV 70 mg vial
caspofungin acetate 50 mg vial
caspofungin acetate 70 mg vial
ERAXIS 50 mg vial
ERAXIS 100 mg vial
micafungin 50 mg/50 mL – 0.9% NaCl
micafungin 100 mg/100 mL – 0.9% NaCl
micafungin 150 mg/150 mL – 0.9% NaCl
micafungin 50 mg vial
micafungin 100 mg vial
MYCAMINE 50 mg vial
MYCAMINE 100 mg vial
VABOMERE 2 g vial
ZERBAXA 1.5 g vial
Gainwell Technologies handles PA requests for drugs billed through the POS venue. If you are a Mississippi Medicaid prescriber, please submit your PA requests through the Gainwell provider web portal (preferred route) or fax completed PA forms to 866-644-6147. The phone number for the Gainwell Pharmacy PA Unit is 833-660-2402.
7/31/2025
Survey open for public input on development of Rural Health Transformation Plan
On July 3, Congress passed via the FY 2025 budget reconciliation process H.R.1, the One Big Beautiful Bill Act (OBBBA), and on July 4, the President signed it into law. Section 71401 of the Bill modifies Section 2105 of the Social Security Act and establishes a $50 billion grant program ($10 billion per fiscal year for FY 2026 – 2030) for the Department of Health and Human Services (HHS) to distribute payments to the 50 states through the Rural Health Transformation Program. Applications to participate in the grant program must be approved by the HHS Secretary no later than December 31, 2025.
The Office of the Governor, in coordination with the Mississippi Division of Medicaid (DOM) and the Mississippi State Department of Health (MSDH), intends to solicit public input through a public survey and a stakeholder forum to develop a Rural Health Transformation Plan (Plan), and submit a timely application for the grant funding. The Office of the Governor will make the final selection for initiatives included in the Plan.
Please complete the survey by 5 p.m. on Thursday, Aug. 14, 2025: Rural Health Transformation Program Stakeholder Survey
See the full Survey: https://medicaid.ms.gov/wp-content/uploads/2025/07/Attachment-E-Rural-Health-Transformation-Program-Stakeholder-Survey.pdf
To learn more visit: https://medicaid.ms.gov/rural-health-transformation-program/
7/29/2025
DOM seeks consultant to support Rural Health Transformation Program
The Mississippi Division of Medicaid (DOM), in coordination with the Office of the Governor and the Mississippi State Department of Health (MSDH), is soliciting quotes from consultants to prepare the State’s Application for the Rural Health Transformation Program provided for in The One Big Beautiful Bill Act.
Offers must be submitted by 2 p.m. on Monday, Aug. 4.
In order for the State to qualify for available funding, the State must submit a detailed Rural Health Transformation plan which must be approved by the Administrator of the Centers for Medicare and Medicaid Services (CMS) no later than December 31, 2025.
Potential offerors can read the entire Request for Quotes with detailed instructions at https://medicaid.ms.gov/resources/procurement/.
The successful offeror will be required to work with staff designated by the Governor, the State Health Officer, and the Executive Director of the Division of Medicaid to:
- Attend the Rural Health Transformation Forum on August 22, 2025, in Jackson, Miss.
- Develop a timeline of tasks to be performed in order to meet the submission deadline. The tasks and deadline may be evolving as new guidance is issued by CMS.
- Analyze the data gathered through the survey and forum to create a list of possible uses for any funds allotted to the State of Mississippi no later than August 31, 2025. The list should provide enough information regarding each option so that an informed final decision can be made as to which option(s) will be included in the State’s Rural Health Transformation Plan (“the Plan”).
- Provide weekly written and verbal updates to Office of the Governor, MSDH, and/or DOM staff members on progress toward the goal of submission of the Plan.
- Prepare the Plan and application in accordance with the requirements established by the Administrator of CMS. The Plan may need to be completed in as little as 30 days but no more than 60 days, depending on the timelines established by CMS.
- Provide no less than 30 days for review of the Plan and application by the Governor, the State Health Officer, and the Executive Director of the Division of Medicaid, and to make any required revisions.
- Ensure the Plan and application are timely submitted in accordance with any requirements established by the Administrator of CMS.
7/9/2025
Provider Directory Updates: Keep Your Information Current
In an ongoing effort to maintain the accuracy and integrity of the Mississippi Medicaid Provider Directory, the Division of Medicaid announces critical updates to provider data collection and maintenance procedures.
Effective immediately, all relevant provider information will be collected at the time of initial enrollment, recredentialing, and revalidation through the provider applications. Additionally, providers may update their information at any time via the MESA Provider Portal.
Maintaining accurate provider directory data is essential to ensure Medicaid members have access to current and reliable information. In compliance with the Consolidated Appropriations Act of 2021, all Mississippi Medicaid enrolled providers (including those in Fee-for-Service, MSCAN, and MSCHIP) must review and validate their provider directory information at least every 90 days.
Expanded Provider Information
The information available for updates has been expanded to include several additional data elements related to the servicing location. Providers are encouraged to update the following, where applicable:
• ADA compliance accommodations available at the facility.
| Accommodation | Definition |
|---|---|
| Signage | Clear, accessible signs with visual and tactile elements are provided to help individuals who are blind or have low vision navigate the space easily. |
| Parking | Designated accessible parking spaces are available near entrances, with appropriate signage and enough space for wheelchair access. |
| Building Exterior | Entrances have ramps or automatic doors, and pathways should be wide and well-maintained to accommodate mobility devices. |
| Building Interior | Hallways and doorways are wide enough to allow for wheelchair passage, and there are accessible routes to all essential areas. |
| Restroom | Restrooms are equipped with grab bars, sufficient space for maneuverability, and features that are easy to operate. |
| Exam Room | Exam rooms have enough space for wheelchair access. |
| Wheelchair Weight Scale | Wheelchair weight scales are available to allow individuals to weigh themselves without transferring from their wheelchairs. |
| Exam Table | Exam tables are height-adjustable to facilitate easy access for individuals with different mobility needs. |
| Patient Lifts | The location has patient lift(s) to safely transfer a patient from a wheelchair to the exam table. |
| Radiologic Equipment | Radiologic equipment for individuals with physical disabilities is available. |
| Public Transportation Access | Location is near accessible public transportation options, with clear paths from transit stops to the building. |
| Gurneys/Stretchers | An accessible gurney (a table on wheels) or stretcher is available and can be lowered to the height of the patient’s wheelchair seat and raised to transfer the patient safely onto an exam table or other surface. |
• Availability of telehealth services.
• Digital contact information (endpoints) for direct electronic communication (learn more).
• Electronic prescriptions, if applicable.
• If a Referral is required, if applicable.
• Office Hours
• Accepting New Patients
How to Update Your Information
1. Access & Log in to MESA Provider Portal
• Visit the MESA Provider Portal and log in with your credentials.
2. Update Characteristics
• Navigate to “Characteristics” under the Provider section in the sidebar.
• Click the plus (+) icon next to Addresses to view your Corporate, Mail To, Pay To, or Servicing Address (Note: Servicing Address cannot be edited).
• Scroll down, click “Edit” to make changes, then “Save” to submit.
3. Add or Modify Languages
• Click the plus (+) icon next to “Languages” and Add/Remove as needed.
• Select from the dropdown to Add or click “Remove” in the Action column to delete a language.
• All updates are saved automatically.
4. Update Coordinated Care Organization (CCO) Selection
• Click the plus (+) sign next to CCO Selection.
• Select or deselect the appropriate CCO(s). Note: This does not replace the contracting/enrollment process with the CCO.
• Click “Submit” to save.
Need Help?
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/05/Q2-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County_v2.0.pdf.
Accurate, up-to-date provider information ensures that Mississippi Medicaid members can make informed decisions about their healthcare. Your cooperation is greatly appreciated.
7/3/2025
834 processing delays to be resolved
The Mississippi Division of Medicaid, Gainwell, and the CCOs are aware of an issue that occurred with some member assignments to the CCOs via the 834 processes. This issue impacted 1,234 members and is causing some provider PA processing delays by the CCOs. Gainwell is currently working to resolve the issue and to generate new 834s to the CCOs as soon as possible. We apologize for any issues this has caused and are working diligently to resolve the matter.
7/2/2025
Updated EDI Companion Guide now available
The Mississippi Division of Medicaid has made updates to its Health Care Eligibility Benefit Inquiry and Response (270/271) Companion Guide, which can be found along with all other EDI Companion Guides at: https://medicaid.ms.gov/edi-technical-documents/.
6/26/2025
Reprocessing Dental Claims for Error Codes 5662, 5660, 5661 and 5613
The Mississippi Division of Medicaid will reprocess and adjust dental claims for alveoloplasty procedure codes denied with error codes 5662, 5660, 5661 and 5613.
To prevent these errors from posting in the future, the extraction codes must be billed prior to the alveoloplasty codes. If the tooth extractions and alveoloplasty procedures are billed on the same claim, the extractions must be billed on details prior to the alveoloplasty codes.
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/05/Q2-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County_v2.0.pdf.
6/25/2025
Attention Durable Medical Equipment Providers Receiving Medicare Part B Claim Denials with Edit/EOB 2502
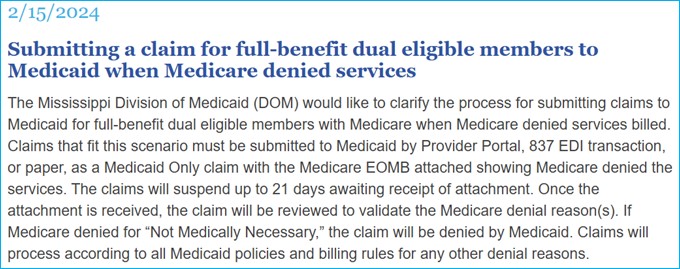
The Division of Medicaid and Gainwell recently updated Medicare Part B system edit 2502 which impacts Durable Medical Equipment (DME) providers. Refer to the previous Late Breaking News article posted on 2/15/2024, (pictured below) clarifying the process for submitting claims to Medicaid for full-benefit dual eligible members with Medicare when Medicare denied services billed. Claims that fit this scenario must be submitted to Medicaid by Provider Portal, 837 EDI transaction, or paper, as a Medicaid Only claim with the Medicare Explanation of Medicare Benefits (EOMB) attached showing Medicare denied the services and the denial reason.
The 837 EDI transaction claims will suspend up to 21 days awaiting receipt of attachment. Claims and EOMB attachments will be reviewed to validate the Medicare denial reason(s). If Medicare denied for “Not Medically Necessary,” the claim will be denied by Medicaid. Claims will process according to all Medicaid policies and billing rules for any other denial reasons.
For Medicare Crossover claims submitted via the EDI X12 (electronic submission), the provider must create a unique Attachment Control Number (ACN) for each claim. The ACN must be entered in the ‘PWK06’ segment of the transaction. Also, a value of ‘BM’ (for By Mail) must be entered in the ‘PWK02’ segment. A Claim Attachment Form must accompany each EOMB and must identify the Provider NPI, Attachment Control Number (ACN) as it was entered in the PWK segment, Claim ID/ICN and Member ID Number. The Claim Attachment Form is located at: https://medicaid.ms.gov/resources/forms/
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/05/Q2-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County_v2.0.pdf.
6/25/2025
UnitedHealthcare Community Plan of Mississippi market departure
The following is an announcement to the provider community from UnitedHealthcare Community Plan.
We regret to inform you that UnitedHealthcare Community Plan (“UnitedHealthcare”) will not be a Mississippi Health Care Programs option for members effective July 1, 2025. This includes the following health plans:
• Coordinated Access Network Program (MSCAN)
• Children’s Health Insurance Program (CHIP)
Members have been notified
We remain committed to our members and to you as one of our participating care providers. UnitedHealthcare members impacted by this change were notified and assigned a new health plan by the Mississippi Division of Medicaid to ensure a smooth transition of care.
Who’s not affected
If you’re a contracted care provider for UnitedHealthcare for Commercial HMO, PPO or POS and Medicare Advantage (including DSNP), this change does not affect members under those plans. However, UnitedHealthcare will no longer serve members under Mississippi CAN and CHIP Programs effective July 1, 2025.
Member care
We’ll continue to provide member care until June 30, 2025. Please use the following guidelines during this transition:
Eligibility and benefits – Continue to verify member eligibility every time a member seeks care.
Claims submission – Continue to submit claims for eligible members with dates of service up to and including June 30, 2025. UnitedHealthcare will remain responsible for all medically necessary services rendered to our members through June 30, 2025, at 11:59 p.m. Effective July 1, 2025, the new health plan will be responsible for the members’ care, claims and authorizations unless a member is at an inpatient facility and is expected to remain past June 30, 2025.
Note: Please ensure that all claims are submitted for payment within 180 days of the date of service or date of discharge.
Member questions – Members can still reach out to us using the phone number on the back of their ID card. Our member services team will continue to be available to assist with their questions.
Continuity of care – Please call the member’s new managed care organization (MCO) beginning July 1, 2025, to better understand their continuity of care procedures. UnitedHealthcare coverage for all members ends June 30, 2025, unless a member is at an inpatient facility and is expected to remain past June 30, 2025. In those cases, UnitedHealthcare will continue to administer the inpatient members’ benefits through discharge.
Disputes and appeals – Our care provider dispute and appeals process and member appeals and grievances process will remain the same.
• UnitedHealthcare care providers: Please consult your contract and the UnitedHealthcare Community Plan of Mississippi Care Provider Manual at UHCprovider.com > Coverage and payments > Administrative guides and manuals > Community Plan Care Provider Manuals for Medicaid Plans by State for information on provider and member appeals and grievances
We’re here to help
To help make this transition easier for you, UnitedHealthcare remains committed to providing support for our care provider network after the contract end date of June 30, 2025.
• UnitedHealthcare care providers: You can continue to access UHCprovider.com for information and support
Thank you for your partnership and for your care to our UnitedHealthcare Community Plan of Mississippi members.
6/24/2025
Training Required for E&D Providers of ADC, PCS, & IHR
Providers of Elderly and Disabled (E&D) Waiver services must satisfy all requirements set forth in Title 23 Miss. Admin. Code Part 208, newly revised effective June 1, 2025.
To ensure all providers are educated on these requirements, the Office of Long Term Services and Supports has scheduled Mandatory Training on Friday, June 27, 2025 for providers of Adult Daycare (ADC), Personal Care (PCS), & In-Home Respite (IHR).
This training should be attended by the agency Owner, Administrator, and/or Compliance Officer but must be attended by an individual with signature authority for the agency.
Please review the agenda here and use the below link to register for the training.
E&D Waiver Provider Training RSVP
6/24/2025
CMS Alert: Medicare Fraud Scheme Involving Phishing Fax Requests
The Centers for Medicare & Medicaid Services (CMS) has identified a fraud scheme targeting Medicare providers and suppliers. Scammers are impersonating CMS and sending phishing fax requests for medical records and documentation, falsely claiming to be part of a Medicare audit.
Important: CMS doesn’t initiate audits by requesting medical records via fax. Protect your information. If you receive a suspicious request, don’t respond. If you think you got a fraudulent or questionable request, work with your Medical Review Contractor to confirm if it’s real.
6/23/2025
Possible Increase in Prior Authorization Related Claim Denials – Week of 6/16-6/20
Providers who received prior authorization claim denials for authorizations approved by Telligen during the week of June 16, 2025-June 20, 2025, are advised to resubmit impacted claims beginning Monday, June 23, 2025. There were technical difficulties with Telligen’s submission of the prior authorization data to MESA. The technical issues have been resolved as of 6/20/2025.
Providers who submit requests to Telligen via Qualitrac can also check case status within the Qualitrac portal. Visit Telligen’s Mississippi UM/QIO website to access the Qualitrac portal login at https://msmedicaid.telligen.com or call Telligen directly at 1-855-625-7709 for assistance.
6/18/2025
Reprocessing of Healthier Mississippi Waiver (HMW) Related to Crossover Claims Denied with Error 4371/EOB 1379 and Error 4374/1378
The Mississippi Division of Medicaid (DOM) and Gainwell continue to reprocess Inpatient, Professional, and Outpatient Crossover claims that have a Healthier Mississippi Waiver (HMW) benefit plan, and the claims denied with errors 4371 or 4374. The impact involves claims being denied due to the claim type associated with the member’s benefit plan, which predominantly affects members enrolled in the HMW benefit plan and have Medicare coverage. The reprocessed claims will appear on future remittance advices (RAs).
6/18/2025
Processing Prior Authorizations and Appeals during the transition of Managed Care Organizations
Beginning July 1, 2025, United Healthcare (UHC) will no longer serve as a Managed Care Organization (MCO) for Mississippi Division of Medicaid (DOM). All DOM beneficiaries enrolled with UHC will be disenrolled on 6/30/2025 and will be transferred to a new MCO or to Fee for Service, depending on the member’s choice. Please check MESA to verify all eligibility.
Please see significant dates regarding Prior Authorization and MCO Appeals
Important Notice for Prior Authorizations
All prior authorization requests for dates of service starting 7/1/2025 should be directed to the beneficiary’s assigned MCO. UHC will not be able to provide a review or decision on these services.
Important Notice for Appeals – Action Required
If you are submitting an appeal for a service that you have not completed, please be aware of the following deadlines to ensure the beneficiary’s appeal is reviewed while still eligible with UHC:
- • Standard Pre-Service Appeals must be received no later than June 17, 2025
• Expedited Pre-Service Appeals must be received no later than June 27, 2025
Being attentive to these dates when submitting an appeal will ensure timely review and continued eligibility. After these dates, all Pre-Service Appeals should be filed directly with the newly assigned MCO. We’re committed to working together to make this change as smooth as possible.
5/28/2025
Outpatient Hospital Drug Coverage: J9309 – INJ, POLATUZUMAB VEDOTIN 1MG
Outpatient Hospital Drug Coverage: J9309 – INJ, POLATUZUMAB VEDOTIN 1MG has been opened for coverage in the Outpatient Hospital setting for dates of services on or after 7/1/2024. Providers are encouraged to resubmit claims that were previously denied.
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/05/Q2-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County_v2.0.pdf.
5/23/2025
License Renewal with the Division of Medicaid
In compliance with 42 CFR § 455.412, the Mississippi Division of Medicaid (DOM) is required to maintain up-to-date licensure documentation for all enrolled providers, including those participating in fee-for-service, MississippiCAN, and CHIP programs.
To prevent deactivation of Medicaid provider numbers and interruption in claims payments, providers must submit current licensure information promptly.
With a high volume of licenses set to expire on June 30, 2025, it is strongly recommended that providers submit renewed licenses as soon as possible to ensure sufficient processing time and avoid any potential disruptions in payment.
Who Is Affected?
Although not an exhaustive list, providers holding licenses issued by the following Mississippi state boards may be affected:
- • Mississippi State Board of Medical Licensure
• Mississippi State Board of Physical Therapy
• Mississippi Board of Chiropractic Examiners
• Mississippi Board of Psychology
• Mississippi State Department of Health
License Expiration Notifications
Providers whose licenses are expiring will receive letters of notification by mail from Gainwell Technologies. As noted in the December 30, 2024, Late Breaking News article, the notification will also be available for viewing in the provider portal.
To stay informed, DOM encourages providers to check the Provider Six-Month License Due List, available and updated monthly on the DOM website: View the Provider License Due List
How to Submit Updated Licenses
Licenses should be submitted electronically via the MESA Provider Portal: Access the MESA Provider Portal
(Use the Secure Correspondence feature. A tracking number will be provided upon submission.)
For any assistance required between 8 a.m. and 5 p.m. CST, providers can contact the Provider and Beneficiary Services Call Center at (800) 884-3222.
5/19/2025
How to Enroll/Contract with TrueCare Based on Enrollment with DOM
As previously communicated through Late Breaking News and Provider Bulletins, TrueCare will join Molina and Magnolia as a Coordinated Care Organization (CCO) serving Mississippi Medicaid members, effective July 1, 2025. At that time, UnitedHealthcare will no longer provide coverage for Mississippi members (members will be able to select a new CCO).
Enrollment with TrueCare varies depending on your credentialing agency. This article outlines the appropriate steps for each credentialing scenario to assist you in joining the TrueCare network and beginning service delivery. Click here to learn how to enroll/contract with TrueCare based on enrollment with DOM.
5/14/2025
Reprocessing Crossover Claims Reduced for a Medicaid Cap Calculation
The Mississippi Division of Medicaid will reprocess claims that previously paid with a reduced amount due to a crossover coinsurance and deductible Medicaid cap reduction calculation. The reprocessed claims will appear on your Remittance Advice beginning on 5/19/2025 through the next four weeks.
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/05/Q2-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County_v2.0.pdf.
5/7/2025
TrueCare Orientation Announcement
The following is an announcement to the provider community from TrueCare.
TrueCare is excited to announce our upcoming Provider Orientation sessions!
In anticipation of the TrueCare product launch, we are offering a variety of convenient orientation options designed to better meet your needs. Our Provider Orientation focuses on the collaborative processes that support us working with you. Please prioritize completing orientation prior to July 1, 2025.
Right Click link below and open Hyperlink
Register for Live or Virtual Training: For your convenience, we will offer in-person and virtual sessions. Go to https://healthplanresources.com/learn/course/74/truecare-provider-orientation?generated_by=13055&hash=31f727bf5548d2474db79d9697f322813fd1e55b to register.
All sessions will be held 10:00 a.m. to 12:00 p.m., Central Time (CT).
| May 14, 2025 | USM Long Beach Campus | North Academic Building, NAB 102 730 East Beach Blvd. Long Beach, MS 39560 |
| May 16, 2025 | Baptist Hospital – DeSoto | North Entrance, DeSoto Rooms 7601 Southcrest Parkway Southaven, MS 38671 |
| Live Virtual Sessions | ||
|---|---|---|
| May 19, 2025 | May 20, 2025 | May 21, 2025 |
Can’t Join Us In-Person? For any provider who is unable to attend, training sessions will be recorded and posted to HealthPlanResources.com. You may also view our on-demand presentation. Go to HealthPlanResources.com and select TrueCare Provider Orientation.
Questions? Contact TrueCare at MS_Network@CareSource.com
5/5/2025
Physician Administered Drugs: Prior Authorization Requirements
Effective July 1, 2025, the Mississippi Division of Medicaid (DOM) will require prior authorization (PA) of the following physician administered drugs (PADs):
HCPCS Description
J0178 Injection, aflibercept 1 mg
J2358 Injection, olanzapine, long acting, 1 mg
J2801 Injection, risperidone (rykindo), 0.5 mg
J1306 Injection, inclisiran, 1 mg
J0225 Injection, vutrisiran, 1 mg
J0222 Injection, patisiran, 0.1 mg
J3032 Injection, eptinezumab-jjmr 1 mg
J1427 Injection, viltolarsen, 10 mg
J2356 Injection, tezepelumab-ekko, 1 mg
J0791 Injection, crizanlizumab-tmca, 5 mg
The following code will no longer require PA, effective July 1, 2025.
J9305 pemetrexed, not otherwise specified, 10 mg
Telligen is responsible for authorization requests for fee-for-service (FFS) Medicaid beneficiaries. Please refer to Telligen’s website at https://msmedicaid.telligen.com/, or call Telligen directly at 1-855-625-7709 for assistance. To submit authorization requests, providers are encouraged to register for access to Telligen’s provider portal, Qualitrac, by completing the Telligen Provider Portal Registration.
5/5/2025
Reprocessing Secondary Claims that Denied with Edit 798
The Mississippi Division of Medicaid will reprocess claims denied for edit 798 with the following EOB message: 0798 – TPL – PAYMENT IS LESS THAN PERCENTAGE SPECIFIED ON SYSTEM PARAMETER. The reprocessed claims will appear on your Remittance Advice dated 5/12/2025.
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/04/Q2-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County.pdf.
5/2/2025
April Provider Bulletin now available
The April issue of the MS Medicaid Provider Bulletin is now available online for read or download. The Provider Bulletin aims to inform providers of Medicaid news, policy changes, and provides contact information for provider field representatives listed by county, and more.
Previous issues of the Provider Bulletin are archived online at https://medicaid.ms.gov/providers/provider-resources/provider-bulletins/.
5/2/2025
Mississippi Medicaid Preferred Diabetic Supplies List (DSL)
Effective, July 1, 2025, all OneTouch blood glucose test strips and meters manufactured by LifeScan will be removed from the DSL.
Please refer to the updated DSL at this link MS-Diabetic-Supplies-PDL-5-1-2025.pdf
The Division of Medicaid is providing this courtesy notice to allow providers time to adjust their inventory.
4/25/2025
SFY22 Physician Administered Drug (PAD) Retro Adjustment
The Mississippi Division of Medicaid (DOM) has reprocessed claims with dates of service July 1, 2021, through June 30, 2022, affected by the Physician Administered Drug (PAD) Retro Rate Adjustment. Please refer to the original provider notification dated 3/31/2023 “Mass Adjust Claims Affected by PAD SFY22 Retro Rate” Late Breaking News article. This mass adjustment will appear on your remittance advice dated 4/28/2025.
Per Administrative Code, Part 200, Rule 1.8, providers have 90 calendar days to request an Administrative Review from the date of the denial when DOM adjusts claims after timely filing and timely processing deadlines have passed (Timely Filing Review Request).
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/04/Q2-2025-PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County.pdf.
4/16/2025
Special Enrollment Period for Managed Care Members
What is Special Open Enrollment?
- • Special Open Enrollment a time frame designated for Medicaid members to make a one-time change to their plan prior to the operational phase of a new contract and its Coordinated Care Organizations (CCOs).
When is Special Open Enrollment?
- • Special Open Enrollment is from March 2025 to June 1, 2025.
What has changed with Managed Care?
- • UnitedHealthcare Community Plan will no longer provide health coverage for the MississippiCAN and CHIP program after June 30, 2025.
- • Starting July 1, 2025, Molina Healthcare, Magnolia Health, and TrueCare will provide managed care coverage for both the MississippiCAN program and CHIP.
What happens to UnitedHealthcare members?
- • Members who are currently enrolled with UnitedHealthcare will remain with the plan until June 30, 2025.
- • Letters will be mailed to all managed care members. Each member will have the choice to select one of the three CCOs.
- • UnitedHealthcare members that do not return their enrollment form by June 1, 2025, will be assigned to one of the three CCOs (Magnolia, Molina, or TrueCare).
Will UnitedHealthcare members that do not complete an enrollment form be assigned to TrueCare only?
- • No. UnitedHealthcare members will be assigned to all three CCOs.
Current Managed Care CCOs:
| Mississippi Coordinated Access Network (MississippiCAN) |
Children’s Health Insurance Program (CHIP) |
|---|---|
| Magnolia Health | Molina Healthcare |
| Molina Healthcare | UnitedHealthcare Community Plan |
| UnitedHealthcare Community Plan |
Managed Care CCOs Effective July 1, 2025:
| Mississippi Coordinated Access Network (MississippiCAN) |
Children’s Health Insurance Program (CHIP) |
|---|---|
| Magnolia Health | Magnolia Health |
| Molina Healthcare | Molina Healthcare |
| TrueCare | TrueCare |
How can a member switch plans during open enrollment?
• Members may switch CCOs by:
o Returning enrollment forms by mail, in the postage paid envelope provided in the packet
o Fax a copy of the form to 1-866-644-6050
o Online Portal: http://medicaid.ms.gov/mississippican-enrollment/
• Members may only switch once and will not be able to change health plans until Open Enrollment 2026.
What if the member calling does not receive a Special Open Enrollment Letter?
• Check their mailing address and have them update their mailing address and telephone number.
• Forward calls for enrollment forms to:
| Contact | Telephone |
|---|---|
| Gainwell (Enrollment Broker) | 1-866-644-6050 |
| Managed Care Eligibility | 601-359-3789 |
3/10/2025
Gloves and Wipes for Incontinence
Effective 1/1/2025 the Mississippi Division of Medicaid will cover non-sterile gloves and disposable sanitary wipes utilized for incontinence care of members aged three (3) and above, when deemed medically necessary. HCPCS code A4927 should be used when billing for non-sterile gloves and HCPCS code A9286 for disposable sanitary wipes. The code for disposable wipes (A9286) requires a manual pricing process by Gainwell and will reimburse at $0.12 per wipe. Documentation of MSRP must be submitted with claims for wipes.
Please refer to the Division’s Administrative Code Part 209 Durable Medical Equipment and Medical Supplies , Rule 2.2: Covered Medical Supplies, AA. Incontinence Garments and Supplies for details at the following link Administrative Code.
3/5/2025
Register Now for Telligen March 2025 Training Sessions
Please review the session descriptions below and use the registration links provided to select the most relevant options for your needs. During these training sessions, Providers will:
- • Learn the step-by-step process for submitting prior authorization requests, including required documentation and deadlines.
• Understand discharge submission procedures and how to verify eligibility.
• Gain clarity on the appeals process for denied requests and enhance your navigation of the Telligen Provider Portal
1. General Monthly Qualitrac Q&A
This session is a general introduction to Qualitrac and is open to all users. It provides an overview of Qualitrac navigation, authorization submission, and common troubleshooting steps. Attendees will gain a better understanding of documentation requirements, eligibility verification, and the appeals process. The session will also discuss updates and enhancements in the Qualitrac provider portal. A Q&A session will follow to address any questions. These sessions are held monthly and are optional to attend.
2. Review Type: Therapy (ST,OT,PT)
This training is specifically catered to providers who submit Therapy (ST, OT, PT) review types, including Speech, Occupational, and Physical therapy. The session will educate providers on the proper authorization process, review required documentation (including treatment plans and progress notes) and explain Medicaid coverage and eligibility requirements for therapy services. Providers will be guided on submitting requests through Qualitrac, selecting appropriate review types, and handling common denials and appeals. A Q&A session will follow to address any questions. Specific Review Trainings are offered at two different times for your convenience, but you only need to attend one session per topic.
3. Review Type: Behavioral Health
This training is specifically catered to providers who submit Behavioral Health review types, including inpatient psychiatric services, outpatient mental health, and substance use disorder treatments. The session will provide a comprehensive review of the authorization process, including documentation requirements, psychiatric evaluations, and treatment plans. Providers will be guided on submitting prior authorizations, responding to requests for additional information, and navigating the appeals process, including reconsiderations and peer-to-peer reviews. A Q&A session will follow to address any questions. Specific Review Trainings are offered at two different times for your convenience, but you only need to attend one session per topic.
Please use the registration links provided below to secure your spot in the session(s) of your choice.
Session 1: March 11, 2025, 2:00 PM CST Monthly Qualitrac Q&A
Session 2: March 13, 2025, 10:00 AM CST Therapy Review Training Session 1
Session 3: March 20, 2025, 2:00 PM CST Therapy Review Training Session 2
Session 4: March,25 2025, 2:00 PM CST Behavioral Review Training Session 1
Session 5: March,27 2025, 10:00 AM CST Behavioral Review Training Session 2
For assistance, please contact Telligen’s Customer Service at: 1-855-625-7709 or via email at msmedicaidum@telligen.com. Visit Telligen’s Mississippi UM/QIO website to register for portal access https://msmedicaid.telligen.com.
3/3/2025
Join the TrueCare Network
TrueCare is a Mississippi-based, non-profit, provider-sponsored health plan formed by a coalition of hospitals and health systems across the state. Backed by CareSource’s national expertise in quality and operational excellence, TrueCare offers locally based provider services through dedicated provider engagement representatives and customer support.
How to Begin the Contracting Process
Online:
- Visit the TrueCare website at MSTrueCare.com.
- Click “Join Our Provider Network.”
- Locate the blue box and click “Start a Contract.”
- Under Request Type, select New Contract.
- Under Product Type, choose MS Medicaid – TrueCare.
- Complete the Submitter Information and Contract Signatory Information sections.
- Add your providers/locations.
- Attach all required documentation.
- Click Submit.
- You will receive an auto-generated confirmation email upon submission.
Offline:
To request a contract by email, contact:
- Shelia Reed at Shelia.Reed@caresource.com
- Trisha Southerland at Trisha.Southerland@caresource.com
A contract will be sent to you for completion and return. For more information, visit MSTrueCare.com.
2/26/2025
Mississippi Outcomes for Maternal Safety (MOMS) Initiative – Outpatient Provider Training: OB/GYN Physicians
The Mississippi Division of Medicaid (DOM) is hosting a webinar to help OB/GYNs and postpartum providers understand the new MOMS Initiative, a value-based payment program aimed at improving maternal health.
The webinar will provide an overview of the VBP program, including:
- • MOMS Risk Assessments and Postpartum Follow-up Requirements
• Best Practices in Postpartum Care
• Incentive Payment Structure
• Provider Support Resources.
Physicians and outpatient providers can earn a $250 incentive for each managed care patient who completes a postpartum follow-up visit within the timeframe based on their MOMS risk score. CCOs and DOM will track these visits using administrative claims data and the TS modifier (optional but recommended for accurate reporting).
Timely postpartum follow-up is essential for preventing complications, reducing hospital readmissions, and ensuring appropriate postpartum care. The MOMS follow-up visit serves as the initial postpartum visit based on the patient’s assessed risk level but does not replace standard postpartum care.
These incentives aim to improve maternal health outcomes for Medicaid beneficiaries by promoting timely follow-up care and reducing maternal morbidity across the state.
Webinar Details
Date: Wednesday, March 5, 2025 1:00-2:30 p.m. CT
Registration Link: MOMS – OP Provider Training
This webinar will be recorded and made available on the DOM Website – Mississippi DOM VBP
For questions, please contact QIPP@medicaid.ms.gov or David Paradiso at dparadiso@mslc.com.
We encourage all outpatient providers to attend and help improve maternal health outcomes across Mississippi.
2/20/2025
Attention Community/Private Mental Health Center Providers
Please be advised that individuals receiving Home and Community Based Services (HCBS) case management/support coordination (CM/SC) cannot also receive Community Mental Health Services Targeted Case Management (T1017). This is considered a duplicative service by the Centers for Medicare and Medicaid Services. If an individual is locked-in a waiver or Community Support Program (CSP), the HCBS agency is the case management service provider. Should the Community Mental Health Center/Private Mental Health Center become aware of a beneficiary’s need normally handled through TCM, they should contact the beneficiaries’ support coordinator or CSP TCM.
Targeted Case Management claims submitted for individuals with a lock-in will deny with edit 756-MH CASE MGMT NOT ALLOWED FOR HCBS OR CSP MEMBER. Claims that have paid and processed inappropriately will be recouped.
As a reminder, eligibility should be checked each date of service. To determine if a beneficiary is enrolled in a HCBS program go to your MESA provider portal:
- • Select the “Eligibility” tab at the top of the screen, then select “Eligibility Verification”.
- • Enter the “Member ID” or other requested information if Member ID is unknown. Enter an effective from and effective to date (no more than a 30-day span) and click the blue “Submit” button at the bottom left of the screen.
- • Click on “Medicaid State Plan” located at the bottom of the screen under “Benefit Details” and “Coverage”.
- • Click on “Expand All” option above the “Effective/End Dates”.
- • The “Lock-in Details” and “Benefit Plan” are displayed for the date range selected.
- • HCBS Lock-ins are identified in MESA as follows: Assisted Living (WAL), Elderly and Disabled (WED), Independent Living (WIL), Intellectual Disabilities/Developmental Disabilities (WID), Traumatic Brain Injury/Spinal Cord Injury (WTB), or Community Support Program (CSP).
Please refer to Mississippi Division of Medicaid Administrative Code or State Plan Amendment references as follows:
Part 206: Mental Health Services
Chapter 1, Rule 1.2.X and Chapter 1, Rule 1.3.D
Part 208: Home and Community Based Long Term Care Services
Assisted Living (WAL) Waiver Chapter 3, Rule 3.6
Elderly and Disabled (WED) Waiver Chapter 1, Rule 1.6
Independent Living (WIL) Waiver Chapter 2, Rule 2.6
Intellectual Disabilities/Developmental Disabilities (WID) Waiver Chapter 5, Rule 5.5
Traumatic Brain Injury/Spinal Cord Injury (WTB) Waiver – Chapter 4, Rule 4.5
Community Support Program (CSP) Attachment 3.1-A, Exhibit 19b, Page 1 Supplement 1C to Attachment 3.1-A, Pages 1-4
2/13/2025
Marketplace Policies and Medicaid Coverage
Medicaid members are allowed to purchase Marketplace plans. These policies are considered primary, and Medicaid will be the secondary payor. Providers should bill the Marketplace policy prior to billing Medicaid. The original explanation of benefit (EOB) from the Marketplace carrier must be attached to the claim if filing paper or MESA web portal.
Members who are not aware of their Marketplace coverage should be instructed to reach out to the Marketplace carrier to disenroll/cancel the policy. After disenrollment/cancellation of the policy, the member should contact the Office of Recovery at (601) 359-6095 with the termination date and reference number provided by the Marketplace plan. Providers should rebill the claim once the updates are completed in MESA. If you have additional questions, please contact the Office of Recovery at (601) 359-6095.
2/12/2025
Reprocessing of Certain Dental Claims Complete that Denied with Billing Update Error Code 5592 (MA 20854)
The Mississippi Division of Medicaid (DOM) has revised the policy for MESA error code 5592 Dental Lifetime Orthodontics Max Dollar Limit to align with the new lifetime limit of $4620. Claim details processed with an effective date of 10/2/2023 through 12/11/2024 that denied with error code 5592 will be reprocessed. The policy limit for error code 5592 was modified from $4200 to $4620. In addition to the increase in the Dental Lifetime Orthodontia limit, an adjustment was made to paid claims with procedure codes D8080, D8670, and D8020 for dates of service 10/2/2023 through 12/11/2024 to allow for SPA 23-0030 Fee update. The mass adjustment will appear on a remittance advice dated 02/17/2025. No further action on the part of the provider is needed.
Should you need assistance, please contact the Provider and Beneficiary Services Call Center at (800) 884-3222 or use the Provider Field Representative list on Medicaid’s website to identify your designated representative. The Provider Field Representative list includes email addresses and phone numbers for each representative. This resource document is located at https://medicaid.ms.gov/wp-content/uploads/2025/02/2025.02.Q1-2025_PROVIDER-FIELD-REPRESENTATIVES_Map-and-By-County.pdf.
2/11/2025
Attention Dialysis Facility Providers
Effective immediately, immunizations will not be reimbursed separately from the prospective payment system (PPS) rate. Please refer to MS SPA 24-0001 End-Stage Renal Disease (ESRD) Services approved by CMS requiring this change.
1/31/2025
January Provider Bulletin now available
The January issue of the MS Medicaid Provider Bulletin is now available online for read or download. The Provider Bulletin aims to inform providers of Medicaid news, policy changes, and provides contact information for provider field representatives listed by county, and more.
Previous issues of the Provider Bulletin are archived online at https://medicaid.ms.gov/providers/provider-resources/provider-bulletins/.
1/27/2025
Mississippi Outcomes for Maternal Safety (MOMS) Initiative
The Mississippi Division of Medicaid (DOM) is pleased to announce the Mississippi Outcomes for Maternal Safety (MOMS) Initiative. The MOMS Initiative is a value-based payment (VBP) program aimed at enhancing maternal health outcomes across the state. To address Mississippi’s high rates of severe maternal morbidity (SMM), the MOMS Initiative will support redesigned care delivery by incorporating new discharge protocols and requirements for post-discharge follow-up appointments. DOM has initiated and filed a preprint with the Centers for Medicare & Medicaid Services (CMS) to allow incentive payments to maternity hospitals and outpatient providers.
The MOMS assessment evaluates the real-time condition and factors linked to SMM risk of each patient. The MOMS assessment generates a numerical score that assigns the patient to a MOMS risk level ranging from Level 1 to Level 3. Risk levels determine the urgency of the patient’s initial postpartum follow-up visit. Level 1 patients must be seen within 5 days, Level 2 patients within 10 days, and Level 3 patients within 30 days post discharge.
Hospitals play a pivotal role in assessing maternal health risk and identifying patients at heightened risk for adverse outcomes. To qualify for an incentive payment under the MOMS Initiative, for each managed care patient, hospitals will be eligible to receive a $250 incentive when completing a MOMS assessment and sharing the risk score prior to discharge. By integrating this assessment into routine procedures, hospitals contribute to early detection and proactive planning for postpartum care.
Outpatient providers also play a crucial role. To qualify for an incentive payment under the MOMS Initiative, for each managed care patient, outpatient providers will be eligible to receive a $250 incentive when a patient completes a postpartum follow-up visit within the timeframe specified by their MOMS risk score. These follow-up appointments are essential to ensuring that patients receive timely care during the critical postpartum period, reducing the likelihood of complications such as readmissions or emergency department visits. By tying financial incentives to timely follow-up visits, the program helps improve access to postpartum care and encourages providers to adopt practices that address patients’ specific needs based on their risk profiles.
These incentives aim to promote better maternal health outcomes for Medicaid beneficiaries by encouraging comprehensive assessments and timely follow-up care. These measures are critical to reducing maternal morbidity statewide.
We will be conducting a joint training session with the three CCOs to provide an overview of the program, including the MOMS Assessment form, ADT requirements, roles and responsibilities, best practices for discharge planning, and guidance on incentive payment allocation. The training webinar is scheduled for January 28th from 1:00 to 2:30 PM CT.
You can sign up for and access the webinar using the following link: MOMS Initiative Training Webinar
This webinar will be recorded and made available on the DOM Website: https://medicaid.ms.gov/value-based-incentives/
Should you have any questions regarding this new initiative, please send them to: QIPP@medicaid.ms.gov
1/15/2025
Disenrollment Due to Claims Inactivity
In accordance with upcoming requirements to improve the accuracy of provider directories, any enrolled Medicaid provider not appearing on a submitted claim within the past 12 months will be disenrolled, effective February 1, 2025. For further details, please see the Mississippi Administrative Code, Title 23, Part 200, Rule 4.2 (A) 17.
My provider enrollment was just approved, what can I do to ensure I am not disenrolled for claim inactivity?
Newly enrolled providers will have up to one (1) year to appear on a submitted claim before being subject to disenrollment. To prevent disenrollment, providers should submit claims as services are rendered to Medicaid members.
If I have multiple service location enrollments will all locations be disenrolled if only one location does not have any claims activity?
No, only the servicing locations with no claim activity will be disenrolled.
How will I be notified if I am disenrolled?
Each disenrolled provider will receive a notification letter informing them of the disenrollment by mail. As noted in the December 30, 2024, Late Breaking News article, the notification will also be available for viewing in the provider portal.
What can I do if I am disenrolled?
Providers disenrolled due to inactivity may submit an application to re-enroll in the Medicaid program at any time.
For more information, call the Provider and Beneficiary Services Call Center at 1-800-884-3222 or your designated field representative: https://medicaid.ms.gov/wp-content/uploads/2024/03/Provider-Field-Representatives-1.pdf.
1/13/2025
We Want Your Feedback: Help Us Improve the MESA Portal Claims Submission Process
At the Mississippi Division of Medicaid (DOM), we are committed to ensuring that the claims submission process is efficient, user-friendly, and meets the needs of our providers. To achieve this, we need your valuable input.
We want to hear about your experiences with the claim’s submission functionality of the MESA portal. Whether you use the portal regularly or rely on paper submissions, your feedback is essential in identifying challenges and areas for improvement.
Your insights will help us:
- • Understand the pain points you face when using the portal.
- • Prioritize updates and changes to enhance your experience.
- • Streamline the process to save you time and effort.
Please share your feedback and suggestions by emailing us at ProviderFeedback@medicaid.ms.gov. Be as specific as possible, and feel free to include examples of issues or ideas for improvement. Your input will directly influence future enhancements, and together we can make the MESA portal work better for everyone.
Thank you for partnering with us to improve the claims submission experience for all Medicaid providers!
1/3/2025
Attention Ambulatory Surgical Centers
The Division of Medicaid will no longer require Ambulatory Surgical Centers (ASCs) to obtain prior authorization for procedure code G0330. This change is effective for dates of service on and after December 1, 2024.