EDI Enrollment and Testing
The Mississippi Division of Medicaid (DOM) is in the process of implementing a new Medicaid Management Information System (MMIS) – which will include a new Provider Portal – known as MESA: Medicaid Enterprise System Assistance. The new system, going live at the beginning of October, is being developed by Gainwell Technologies.
EDI testing is now underway, and trading partners are asked to enroll as soon as possible to be able to test EDI submissions to MESA.
What you need to do:
Pharmacy Medicaid Fee for Service (FFS) Providers:
- If you are submitting only NCPDP POS transactions, you are NOT required to enroll as an EDI Trading Partner. Gainwell is coordinating with switch vendors to ensure adequate testing prior to go-live.
- Effective 10/1/2022 at 6 a.m., BIN: 025151 and PCN: DRMSPROD will be required to submit Medicaid fee for service pharmacy NCPDP POS claims.
- The MESA Medicaid Provider Portal is an online tool which will allow you the ability to submit pharmacy claims, inquire on claims, verify beneficiary eligibility, review your enrollment status, and perform drug coverage inquiries. To use this online tool you must register via the MESA Medicaid Provider Portal when it becomes available in late September. You are NOT required to enroll as a Trading Partner in any environment to submit claims via the portal.
Non-Pharmacy Medicaid FFS Providers:
- If you are a Provider that will be submitting EDI compliant batch transactions (either EDI HIPAA or NCPDP) you are required to enroll as an EDI Trading Partner.
- If you are a Provider that has a Clearinghouse that will be submitting EDI compliant batch transactions on your behalf, you are NOT required to enroll as an EDI Trading Partner (but please ensure that your trading partner is enrolled as an EDI Trading Partner).
- If you are a Provider that will be submitting via the Gainwell Medicaid Provider Portal (via direct data entry) you are required to register as a Provider via the MESA Production Medicaid Provider Portal when it becomes available Oct. 3. You are NOT required to enroll as a Trading Partner in any environment.
Trading Partners/Clearing Houses:
- If you are a Trading Partner/ Clearinghouse that will be submitting EDI compliant batch transactions (either EDI HIPAA or NCPDP) you are required to enroll as an EDI Trading Partner.
- If you are a Trading Partner / Clearinghouse that will be submitting EDI compliant batch transactions on behalf of a Provider(s), you will need to coordinate association by sharing your newly assigned Trading Partner ID with your Provider(s) after successful enrollment as an EDI Trading Partner.
To enroll as a Trading Partner in the MESA system and set up your account, follow the steps outlined in the Enrollment and Testing Guidelines below, which contain detailed Gainwell instructions:
Enrollment and Testing Guidelines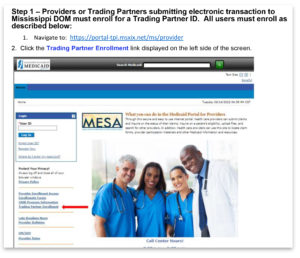
- Trading Partner Enrollment and Register Process
- Trading Partner – Testing Guidelines
- Submission of EDI Transactions Tip Sheet (MOVEit – Multiple file upload/download)
- Submission of EDI Transactions Tip Sheet (Provider Portal – single file upload/download)
- Health Care Portal Access User Account Agreement
These instructions can also be found on the Electronic Data Interchange (EDI) Technical Documents page at https://medicaid.ms.gov/edi-technical-documents/.
DOM Companion Guides
To help you prepare for testing, DOM Companion Guides are now available, which describe the specific technical and procedural requirements for interfaces between DOM and its trading partners. You will have an opportunity to review those companion guides with Gainwell’s technical experts.
If you any questions as you follow the steps for enrollment and registration, please contact Gainwell’s EDI team: MS_EDI_Helpdesk@gainwelltechnologies.com.
PRP-100 (Computer-Based Training) Provider Portal Overview
Access the PRP-100 training course for an overview of the features and functions of the MESA Provider Portal. This training will aid registration, and initial portal navigation. The PRP-100 training course is accessible through the MESA Learning Management System (LMS). Click here and follow the instructions to log into the LMS, as well as a workshop schedule for upcoming training webinars.
You can also view additional MESA information on our website, including FAQs about our transition to our new MMIS. We will update this resource on a regular basis. Please check back frequently!
*This does not apply to CHIP-only providers, as coordinated care organizations currently submit electronic data transactions on their behalf.