The Mississippi Division of Medicaid is working to add new procedure codes that can be used by providers and laboratories to bill for certain Coronavirus Disease 2019 (COVID-19) diagnostic tests to increase the testing and tracking of new cases.
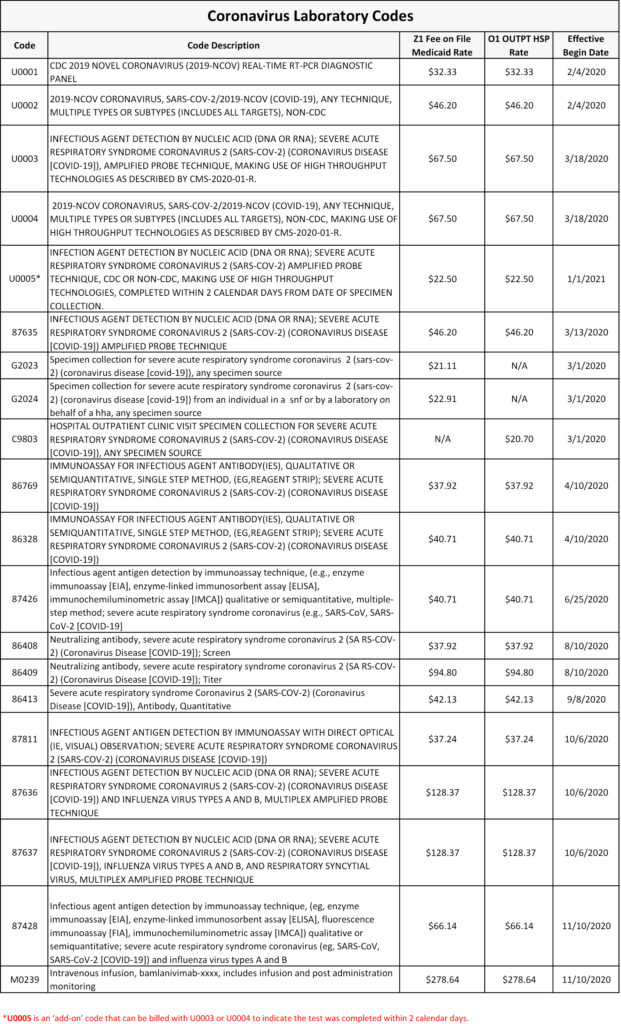
The Healthcare Common Procedure Coding System (HCPCS) codes U0001 and U0002 were developed by the Centers for Medicare and Medicaid Services (CMS). The new Coronavirus Disease 2019 (COVID-19) diagnostic testing codes are now available for billing in the claims processing system and will apply to dates of service on or after Feb. 4, 2020.
The HCPCS code U0001 is specifically used for CDC testing laboratories to test patients for SARS-CoV-2. HCPCS code U0002 allows laboratories to bill for non-CDC laboratory tests for SARS-CoV-2/2019-nCoV (COVID-19). The published fees for the two codes will be:
- U0001 = $32.33
- U0002 = $46.20
These fees do not include cutbacks, assessment fees, etc. Payment is not guaranteed.
For more information on the coverage or the evaluation and testing of COVID-19, find the following resources online:
- Medicaid and CHIP Coverage and Payment Related to COVID-19: https://www.cms.gov/files/document/03052020-medicaid-covid-19-fact-sheet.pdf
- CDC Guidance on Evaluating and Testing Persons for COVID-19: https://www.cdc.gov/coronavirus/2019-nCoV/hcp/clinical-criteria.html
– Published March 16, 2020