Claims
What is timely filing?
As defined in the Mississippi Division of Medicaid (DOM) Administrative Code, a claim is considered timely if it is submitted:
- Within 365 days from the date of service, or
- Within 180 days from the Medicare paid date, whichever is applicable.
Adjustments to Medicaid Fee-For-Service (FFS) claims are permitted within the following timeframes:
- 365 days from the date of the original claim submission, or
- 180 days from the Medicare Paid date, whichever is applicable.
What is the process for claims that have exceeded Timely Filing?
To initiate the review process, providers can complete the Timely Filing Review Request Form available on DOM’s website at www.medicaid.ms.gov or mail the request to
Mississippi Division of Medicaid
Office of Provider Solutions
Attn: Provider Relations
P.O. Box 2222
Jackson, Mississippi 39225
The form can be found under the “Providers” section or accessed directly via the following link: Timely Filing Review Request Form.
All requests must include supporting documentation, including a formal letter that should:
- Describe the issues relevant to the timely filing denial.
- Provide justification for consideration during the review.
In addition, providers must submit all supporting documentation that substantiates the request. Please note that failure to provide all required documentation may result in delays to your review.
Please note that specific documentation requirements are detailed in Part 200, Rule 1.8(B).
Administrative Code References
Providers should review the following sections of the Administrative Code for guidance:
- Part 200, Rule 1.6: Timely Filing
- Part 200, Rule 1.7: Timely Processing of Claims
- Part 200, Rule 1.8: Administrative Review for Claims
- Part 300, Chapter 4: Claim Denials for Policy Regarding Administrative Reviews
The full Administrative Code can be accessed here: Mississippi Medicaid Administrative Code.
How do I know if my procedure code requires a Prior Authorization (PA)?
To determine whether a procedure code requires Prior Authorization (PA), providers can refer to the list available on the Mississippi Division of Medicaid (DOM) website.
To access the list:
- Visit www.medicaid.ms.gov
- Navigate to Home > Providers > Procedure Code PA Requirement, or
- Access the list directly via the following link: Procedure Code PA Requirement – Mississippi Division of Medicaid
The list will display all procedure codes that require prior authorization.
How do I submit a paper claim?
Paper claims must be submitted using the appropriate standardized forms:
- CMS-1500 (02-12) – NUCC standard form for professional claims
- UB-04 (CMS-1450) – NUBC standard form for institutional claims
- ADA-2012 (J430D) – Dental standardized form
All forms should be completed according to the guidelines outlined in the Paper Claims Billing Manual. Please ensure that the provider’s signature and date are included in black or blue ink.
The Paper Claims Billing Manual is available online at the Mississippi Division of Medicaid website. To access the manual, navigate to:
Home > Resources > Paper Claims Billing Manual
or click the following link: Paper Claims Billing Manual – Mississippi Division of Medicaid.
Completed paper claims should be mailed to the fiscal agent at the following address:
Gainwell Technologies
P.O. Box 23076
Jackson, MS 39225
EDI
How to enroll as a trading partner?
Trading partners can enroll through the MESA Provider Portal. To enroll, click on the Trading Partner Enrollment link, complete the required information, select the applicable transaction sets, and agree to the Trading Partner Agreement. The confirmation page provides users their Production Trading Partner ID, temporary MOVEit Password and details upcoming steps. All newly enrolled Trading Partners are required to test within the MESA TPI environment prior to activating the newly enrolled Trading Partner ID for production. Please contact our MS EDI Helpdesk at MS_EDI_Helpdesk@gainwelltechnologies.com to have your test credentials set up.
A detailed job aid outlining the enrollment steps is available on the Mississippi Division of Medicaid website. To access it, navigate to Providers > MESA Portal for Providers, and locate the document titled Trading Partner Enrollment. Alternatively, you can access the page directly here: MESA Portal for Providers – Mississippi Division of Medicaid.
How do I link my trading partner?
Once enrolled, providers can link their trading partner to their provider account within the MESA Provider Portal.
- Providers using an external trading partner or clearinghouse for submitting X12 transactions should follow the instructions in the TPID Linking for Outside Service job aid.
- Providers submitting X12 transactions directly as their own trading partner should refer to the TPID Linking for Self Service job aid.
Both job aids are available on the Mississippi Division of Medicaid website under Providers > MESA Portal for Providers. Look for the respective job aid titled TPID Linking for Outside Service or TPID Linking for Self Service. You can also visit the page directly here: MESA Portal for Providers – Mississippi Division of Medicaid.
Finance
How do I find my Remittance Advice (RA)?
Remittance Advices (RAs) are accessible through the MESA Provider Portal. You can view RAs in one of three ways:
- Within a specific claim
- In payment details
- Under the reports section
A detailed job aid outlining the steps for each method is available on the Mississippi Division of Medicaid website. To access the job aid, navigate to Providers > MESA Provider Portal, then select Financial, and locate the document titled Accessing RAs.
You can also visit the page directly here: MESA Portal for Providers – Mississippi Division of Medicaid.
How do I update my banking information?
Fill out the Direct Deposit Authorization/Agreement Form found on Mississippi Division of Medicaid under Providers by following this path: Forms, Provider Enrollment Forms (expand) and open the Electronic Funds Transfer (Direct Deposit Authorization Form). Also, here is the direct link to forms. Forms – Mississippi Division of Medicaid.
Make one copy of this form for your records and send the form through mail, fax, or secure correspondence with a pre-printed voided check (no starter checks) or bank letter for the account to:
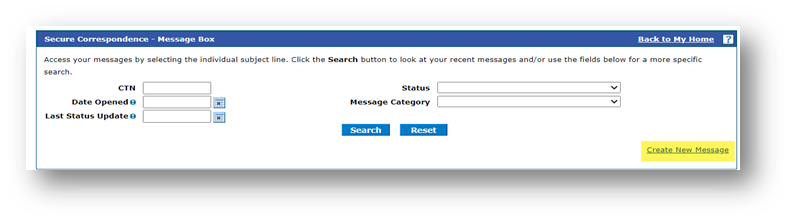
To submit through Secure Correspondence:
Log into your account on the MESA Provider Portal.
Select the Secure Correspondence Link.
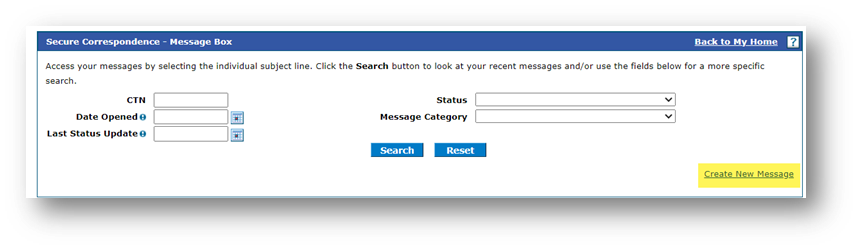
Select Create New Message.
Fill out necessary fields, attach documents, and select Send.
Mail or Fax:
Mississippi Medicaid Program Provider Enrollment
P.O. Box 23078
Jackson, Mississippi 39225
Fax: (866) 644-6148
Provider Enrollment
How do I enroll to be a provider with Mississippi Medicaid?
The enrollment process varies depending on the provider type, but all providers must submit an application online through the MESA Provider Portal.
To begin:
- Visit the Mississippi Medicaid Portal for Providers.
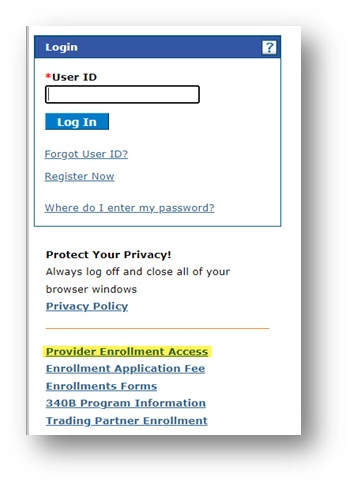
- Select the Provider Enrollment Access link.
- The application will guide you through the required information based on your selected taxonomy and enrollment type.
Enrollment guides for each provider category (including Individual, Group, Facility, Ordering, Referring, Prescribing (ORP), and Other) are available on the Mississippi Division of Medicaid (DOM) website. To access these, navigate to Provider Portal > Provider Enrollment.
How and when do I recredential?
Providers are required to recredential every three (3) years. A recredentialing notice will be sent for each Medicaid ID.
For step by step instructions please view the document titled Provider Recredentialing found on the page MESA Portal for Providers – Mississippi Division of Medicaid under Provider Enrollment.
Failure to complete recredentialing by the due date will result in termination of participation in the MSCAN/MSCHIP programs. Once terminated, the steps to re-enroll depend on your enrolled programs:
- Providers participating in Fee-for-Service (FFS): Must submit an Add Program Application to reinstate participation.
- Providers not participating in FFS: Must submit a new enrollment application.
Does an individual provider have to submit a recredentialing application for each Medicaid ID or portal account?
Individual providers with multiple provider IDs sharing the same NPI will receive a recredentialing notice for each of the provider’s Medicaid IDs. However, recredentialing only one of the IDs will satisfy the requirement for all associated IDs.
If recredentialing is either denied or not completed by the recredential due date, all the individual provider’s enrollments will be terminated, and claims will no longer be payable. To re-enroll in the Mississippi Medicaid program, a new application must be submitted.
Does a facility provider have to submit a recredentialing application for each Medicaid ID or portal account?
Yes, a recredentialing application must be submitted for each service location and corresponding Medicaid ID. Facilities with multiple service locations and provider IDs will receive a recredentialing notice for each provider ID. You must log into your secure portal account and click on the recredential link found under Upcoming Actions. You must log into your Provider Portal account and click on the recredentialing link found under Upcoming Actions to submit the recredentialing application for each ID.
How and when do I revalidate?
In accordance with 42 C.F.R. § 455.414 of the Affordable Care Act (ACA), all state Medicaid agencies must revalidate provider enrollments at least every five years. This ensures that the provider’s credentials, ownership, and other information remain up to date.
Providers will receive a notice when it’s time to revalidate. The revalidation application is available in the provider portal six months before the application is due. Providers can revalidate through the MESA Provider Portal using a step-by-step process. It is crucial to submit the revalidation by the submission date in the notification letter to allow processing time before the deadline.
Failure to complete revalidation by the deadline will result in termination requiring the provider to reapply. To re-enroll in the Mississippi Medicaid program, a new application must be submitted.
If a provider has multiple Medicaid IDs, must each Medicaid ID be revalidated separately?
Yes. Each Medicaid ID must be revalidated separately through its respective provider portal account. Failure to submit a timely revalidation application for any Medicaid ID may result in disenrollment for that specific Medicaid ID, impacting claims and prior authorizations associated with that ID.
How does an organizational provider affiliate to an individual provider working for their organization (link/delink)?
The preferred method is for the provider to link or delink through the MESA Provider Portal, but a request can be sent in writing through mail, secure correspondence on the portal, or by fax. After logging into the secure portal, users can access the affiliated provider information by navigating to: Home > Affiliated Providers. To submit the request to Gainwell Technologies in writing via mail or fax you must list the group Medicaid ID, individual Medicaid ID and the effective date of the link/affiliation.
Gainwell Technologies
Provider Enrollment
P.O. Box 23078
Jackson, MS 39225
Fax #: 866-644-6148
How do I change an authorized official, owner, managing, or directing employee?
The Provider Disclosure Form must be submitted through Secure Correspondence in the MESA Provider Portal. A Change of Ownership (CHOW) Enrollment Application will be required if it meets the requirements outlined in Mississippi Administrative Code Part 200, Rule 4.3.
To access the form:
- Visit the Mississippi Division of Medicaid website.
- Navigate to Providers > Forms.
- Expand the Provider Enrollment Forms section.
- Locate and download the Provider Disclosure Form.
To submit through Secure Correspondence:
Log into your account on the MESA Provider Portal.
Select the Secure Correspondence Link.
Select Create New Message.
Fill out necessary fields, attach documents, and select Send.
What documents are needed for an enrollment application?
The required documentation for an enrollment can be found within the application process on the MESA Provider Portal.
To access:
- Visit the Mississippi Medical Assistance (MESA) Portal for Providers.
- Click on the Provider Enrollment Access link.
- Select the appropriate option for Initial Enrollment, Recredentialing, or Revalidation.
A detailed list of required documents is embedded within each respective application form, guiding providers based on their selected taxonomy and enrollment type.
How do I find my Taxonomy code?
If you are currently a Mississippi Medicaid provider, your assigned taxonomy can be found on the Mississippi Division of Medicaid website under Resources then Taxonomy Look-Up Tool, here is the direct link to the tool: dom-azure-app.medicaid.ms.gov
Note: This is not updated in real time. If you have made recent updates, please allow time for those updates to be made. You are welcome to call Customer Service at 1-800-884-3222 to verify the request was received and updated.
If you are not currently a Mississippi Medicaid provider, please refer to the MESA Taxonomy Listing for a comprehensive list of taxonomies available in Mississippi.
Provider Portal
How do I register for a Web Portal account?
Provider Portal accounts are available only to providers already enrolled in Mississippi Medicaid. You do not need a portal account to submit an enrollment application.
Once enrolled, to register for a portal account:
- Visit the Mississippi Division of Medicaid
- Navigate to Provider Portal > Provider Login.
- Click Register Now and select the appropriate registration option based on your provider type.
How do I set up a delegate for my Portal account?
To add a registered delegate to your account, log in to your MESA Provider Portal and navigate to Manage Accounts under the User Details section.
For step-by-step guidance, refer to the Manage Delegates job aid, available on the Mississippi Division of Medicaid website. To access it:
- Visit the MESA Portal for Providers – Mississippi Division of Medicaid.
- Go to Provider Portal > Provider Enrollment.
- Locate the job aid titled Manage Delegates.
This resource will walk you through the process of adding and managing delegate access.
Third Party Liability (TPL) Carrier Codes
Where can I find Third-Party Liability carrier codes?
A comprehensive list of TPL carrier codes is available on the Mississippi Division of Medicaid website at www.medicaid.ms.gov. To access the list, navigate to the Resources section and select the TPL Carrier Information link.
Note: Claims will not be denied solely based on the use of an incorrect carrier code.