Register Now for Telligen MS UM/QIO Qualitrac Provider Portal Training
As previously announced, the Mississippi Division of Medicaid (DOM) will transition to Telligen, a new Utilization Management/Quality Improvement Organization (UM/QIO), on January 16, 2024.
Beginning Tuesday, January 16, 2024, Telligen will begin performing all new prior authorization reviews for fee-for-service (FFS) Medicaid requests. All authorization reviews submitted prior to January 16, 2024, will be completed by Alliant or Kepro by January 31, 2024. Effective February 1, 2024, all FFS Medicaid authorization related business will be handled by Telligen.
Telligen has prepared the following Provider Training Schedule and invites all Mississippi Medicaid Providers to participate in upcoming virtual training sessions. Training will give Providers a comprehensive overview of Qualitrac, Telligen’s robust portal system for authorization requests. Please use the registration links below to choose the session(s) you wish to attend.
The General Authorization sessions are geared towards providing a general overview of submitting authorizations in our Qualitrac system. The service specific training sessions provide a deeper dive into submitting authorizations for those service types.
REMINDER: Stay tuned for additional upcoming training sessions! Telligen will have more informative sessions planned to further support Mississippi Medicaid Providers in handling authorization requests.
Providers are encouraged to keep an eye on Telligen’s website https://msmedicaid.telligen.com/ for announcements regarding future training sessions. Telligen is committed to providing ongoing learning opportunities to enhance your skills and optimize the care provided to FFS Medicaid beneficiaries.
Should you need assistance, please contact Telligen’s Customer Service at: 1-855-625-7709.
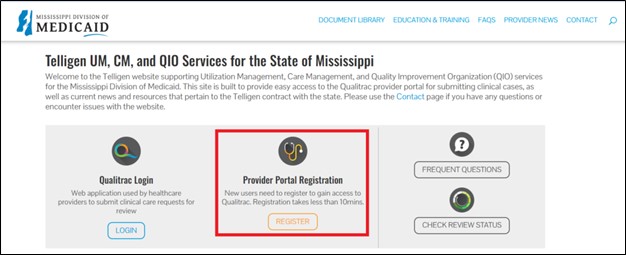
Visit Telligen’s Mississippi UM/QIO website to register for portal access. Look for the Provider Portal Registration option, as indicated in the red box below. https://msmedicaid.telligen.com.
Please note: Prior authorizations for members enrolled in MississippiCAN and CHIP will continue to be handled by the respective coordinated care organization.
– Originally posted on Late Breaking News 12/28/23