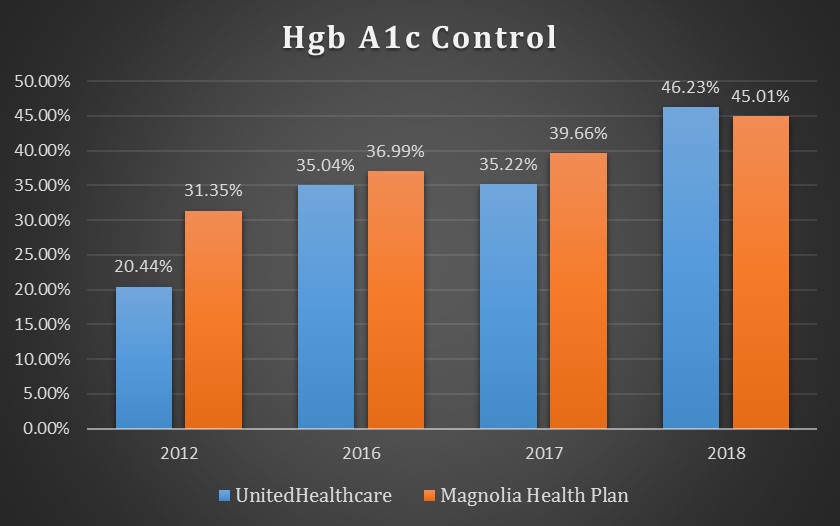
The September 2019 update of the Medicaid Vital Signs dashboard continues to examine how the Mississippi Division of Medicaid’s coordinated care organizations (CCOs) have performed in managing certain common disease states among their members. The CCOs are required to report HEDIS data to the Division on a regular basis. HEDIS, which stands for Healthcare Effectiveness Data and Information Set, is a collection of standardized performance measures developed to compare different managed care plans. This month includes quality measures related to diabetes mellitus and obesity.
At a Glance: Managed Care HEDIS Performance Measures
Diabetes Mellitus
The bar graph above shows the percentages of Medicaid members enrolled with either Magnolia Health Plan or UnitedHealthcare with a diagnosis of diabetes mellitus who received an annual eye exam during the measurement year.
The bar graph above shows the percentages of Medicaid members enrolled with either Magnolia Health Plan or UnitedHealthcare with a diagnosis of diabetes mellitus whose blood-sugar levels were kept in range during the measurement year.
Obesity
The bar graph above shows the percentages of children and adolescents enrolled with either Magnolia Health Plan or UnitedHealthcare with a high body mass index who received weight assessment and counseling for nutrition and physical activity during the measurement year.