The June 2019 update of the Medicaid Vital Signs dashboard expands on previous iterations by taking a look at how the Mississippi Division of Medicaid’s coordinated care organizations (CCOs) have performed in managing certain common disease states among their members. The CCOs are required to report HEDIS data to the Division on a regular basis. HEDIS, which stands for Healthcare Effectiveness Data and Information Set, is a collection of standardized performance measures developed to compare different managed care plans. This month spotlights quality measures associated with diabetes mellitus and hypertension. Additional measures and disease states will be highlighted in future updates.
At a Glance: Managed Care HEDIS Performance Measures
Diabetes
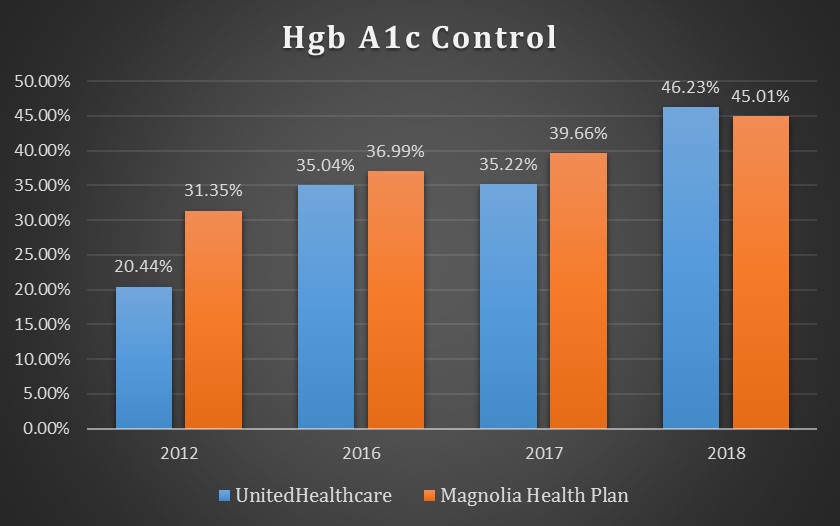
The bar graph above shows the percentages of Medicaid members enrolled with either Magnolia Health Plan or UnitedHealthcare with a diagnosis of diabetes mellitus whose blood-sugar levels were kept in range during the measurement year.
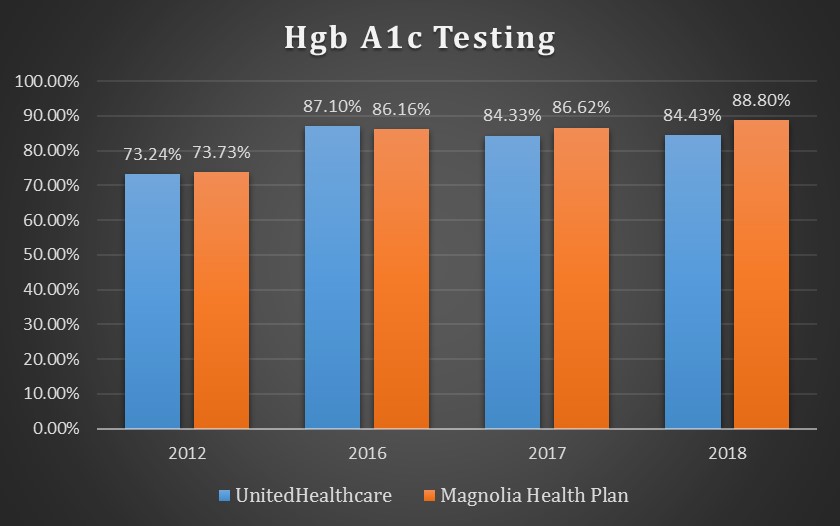
Percentages of Medicaid members enrolled with either Magnolia Health Plan or UnitedHealthcare with a diagnosis of diabetes mellitus and who received an Hgb A1c test during each measurement year.
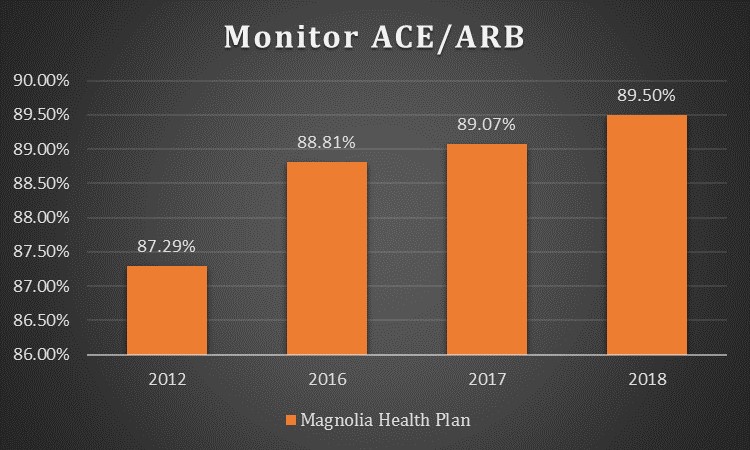
Hypertension
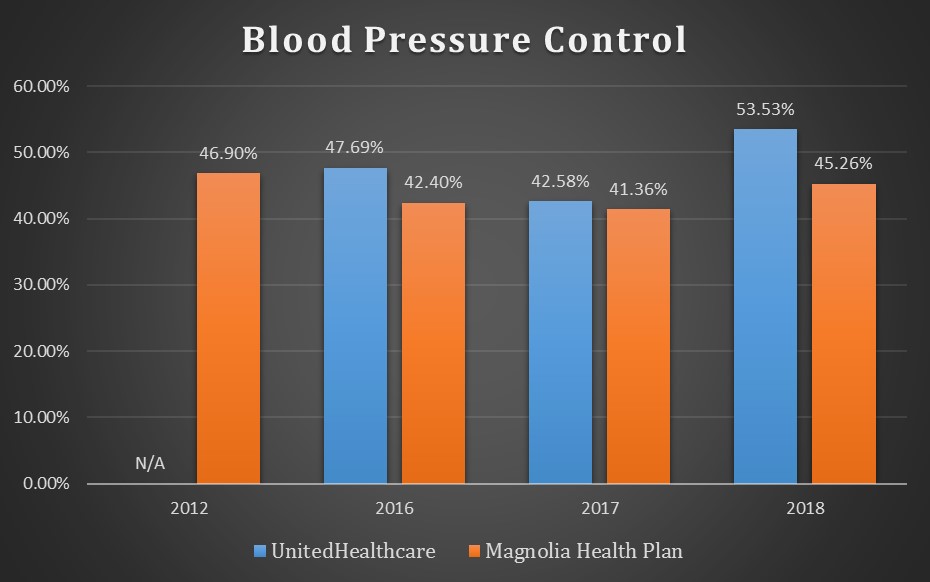 The bar graph above shows the percentages of Medicaid members enrolled with either Magnolia Health Plan or UnitedHealthcare with a diagnosis of hypertension whose blood pressure was effectively controlled during the measurement year.
The bar graph above shows the percentages of Medicaid members enrolled with either Magnolia Health Plan or UnitedHealthcare with a diagnosis of hypertension whose blood pressure was effectively controlled during the measurement year.
Percentages of Medicaid members enrolled with Magnolia Health Plan with a diagnosis of hypertension on multiple medications who were appropriately monitored for preventable adverse drug events during the measurement year. (No data available for UnitedHealthCare.)