Medicaid to implement single Pharmacy Benefit Administrator for all pharmacy claims on July 1, 2024
On July 1, the Mississippi Division of Medicaid (DOM) will implement a single Pharmacy Benefit Administrator (PBA) to streamline and enhance the processing and management of pharmacy claims for all Medicaid members, including those enrolled in MississippiCAN and CHIP.
Operated by Gainwell Technologies, the PBA will also assume all pharmacy prior authorization responsibilities for drugs submitted on pharmacy claims. DOM will continue to require the use of the Universal Preferred Drug List (PDL). This decision comes after careful consideration and evaluation of various factors aimed at enhancing efficiency and transparency in the Medicaid delivery system.
Members should notice no disruption in their care if providers are prepared for this change.
WHAT YOU NEED TO KNOW AND DO
Pharmacy Providers:
Billing Directions
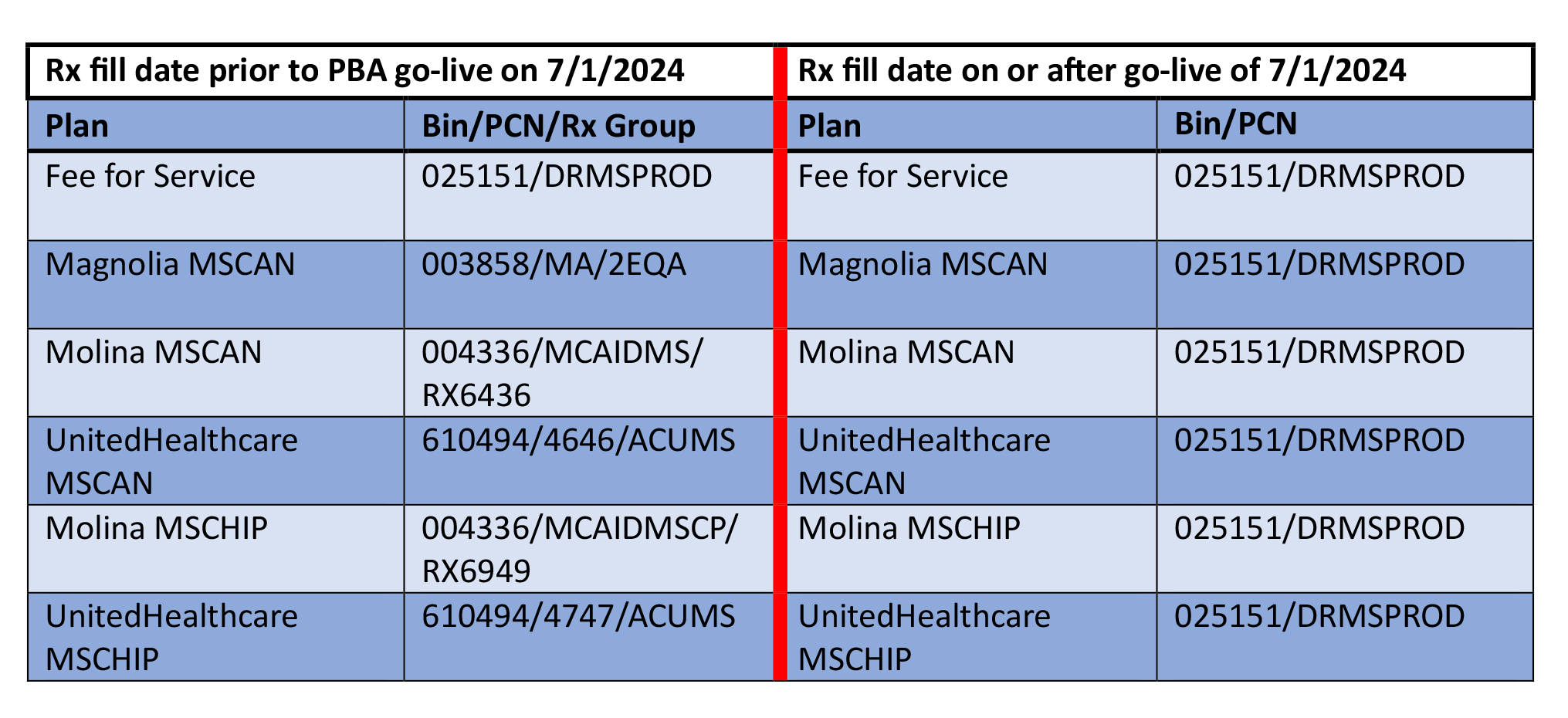
Pharmacy providers must ensure their pharmacy software is configured to submit NCPDP D.0 pharmacy claims, with dates of service of 7/1/2024 and thereafter, for all Medicaid members (fee-for-service-FFS, MSCAN and MSCHIP) to Gainwell using the following billing values:
• BIN – 025151
• PCN – DRMSPROD
Retroactive Billing Directions
To bill pharmacy claims with dates of service prior to 7/1/2024, providers must ascertain which Coordinated Care Organization (CCO) in which the beneficiary was enrolled on that date and submit to that CCO’s PBM. For example, if the member was enrolled with Molina, the claim (s) should be submitted to CVS Caremark. The MSCAN and MSCHIP BIN/PCN values in effect prior to 7/1/2024 should be used. Retroactive billing will be possible for claims with dates of service a year back from 6/30/24.
Claims
To streamline billing for pharmacy providers, all claims will be subject to the same billing rules, regardless of fee for service (FFS), MSCAN or MSCHIP enrollment of the member.
These billing rules will be consistent with the FFS billing rules for claims submitted to GWT prior 7/1/2024.
Medicaid Member ID#
Submit only the first nine (9) digits of the ID Number displayed on the Medicaid card. Do not submit a Person Code.
All Medicaid members receive one of these type of ID cards:
Please note: New plan-specific ID cards have been mailed to members enrolled in MSCAN and MSCHIP plans.
DAW Codes
The only DAW codes recognized in adjudication logic are ‘0’ and ‘7’.
Use of DAW ‘7’ for Narrow Therapeutic Index (NTI) Brand Name Drugs (UPDATE)
Medicaid allows the generic mandate requirement to be overridden for brand name narrow therapeutic index (NTI) drugs to include Coumadin, Dilantin, Lanoxin, Synthroid, and Tegretol.
Pharmacists may now override the generic mandate for NTI drugs by submitting a DAW of ‘7’ on the POS claim for prescriptions on which the prescriber specifies ‘Do Not Substitute’.
Pharmacy Help Desk and Prior Authorization Unit
The Gainwell pharmacy call center phone number is 833-660-2402. This is a direct line to the Gainwell pharmacy help desk to aid with pharmacy claims and pharmacy prior authorizations. All pharmacy claims and prior authorization assistance should be directed to this number.
The GWT pharmacy help desk is open Monday-Friday 8 a.m. – 6 p.m. CST. The GWT help desk is available 24 hours a day, 7 days a week for emergency PA/claims issues.
Prescribing Providers:
DOM requires most prior authorization (PA) requests be signed/submitted by prescribers.
Prescribers and their administrative staff must submit all requests to Gainwell on July 1, 2024, and thereafter. The preferred method of submission is via the MESA Portal for Providers.
PA requests may also be faxed to Gainwell at 866 -644-6147. If PA assistance is needed providers can call 833-660-2402.
General Prior Authorization Instructions can be found on DOM’s website at https://medicaid.ms.gov/wp-content/uploads/2024/07/General-Prior-Authorization-Instructions-7_1_2024.V4-1.pdf.
PA reconsideration requests and appeals can also be sent to Gainwell directly via fax at 866- 644-6147.
In an effort for a smooth transition to the single PBA, GWT has attempted to convert all MSCAN and MSCHIP PAs with approval dates in effect on/after 7/1/2024. In some cases, new PA requests may be required from prescribers.
Link to PAs Forms – https://medicaid.ms.gov/pharmacy-prior-authorization/
Voluntary 90-Day Maintenance Drug List
DOM is in the process of expanding this list. The GWT pharmacy help desk will issue PAs for 90-days supplies for members on a case-by-case basis.
Weekly Remittance Advice (RA) Statements
Pharmacy providers will receive one weekly payment for all claims. FFS, MSCAN and MSCHIP claims will appear on a single, weekly RA from GWT.
Reimbursement change for CHIP claims
MSCHIP claims will be reimbursed using the same methodology used for fee-for-service and MSCAN claims.
Billing of preferred diabetic supplies allowed via pharmacy claims
Effective 7/1/2024, diabetic supplies will be allowed to be billed on pharmacy claims. Diabetic supplies allowed to be billed via pharmacy claims are blood glucose meters and test strips, continuous glucose monitors (CGMs), disposable insulin pumps and components, insulin pen needles and syringes. Please see the MS Medicaid Diabetic Supplies Preferred Product List at https://medicaid.ms.gov/preferred-drug-list/.
Billing via medical claims by DME providers will still be allowed to minimize access issues for members.