How to Enroll/Contract with TrueCare Based on Enrollment with DOM
As previously communicated through Late Breaking News articles and Provider Bulletins, TrueCare will join Molina and Magnolia as a Coordinated Care Organization (CCO) serving Mississippi Medicaid members, effective July 1, 2025. At that time, UnitedHealthcare will no longer provide coverage for Mississippi members (members will be able to select a new CCO).
Enrollment with TrueCare varies depending on your credentialing agency. This article outlines the appropriate steps for each credentialing scenario to assist you in joining the TrueCare network and beginning service delivery.
Credentialed Through DOM
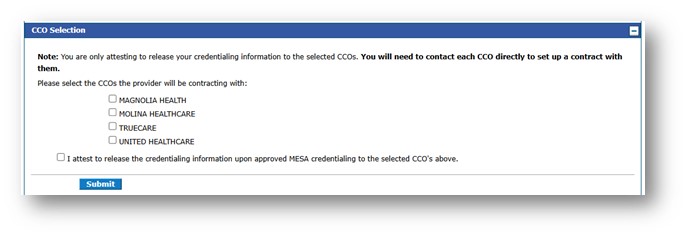
If you provided your CAQH ID during enrollment and were credentialed through DOM, you can update your CCO selections by following these steps:
1. Log into the MESA Provider Portal at https://portal-uat.msxix.net/ms/provider.
2. Update your CCO selections by clicking the Characteristics link.
3. Select the CCO Selection row by clicking the plus sign.
4. Select the CCOs with which you wish to contract and click Submit.
Please note the following important dates:
- UnitedHealthcare will no longer provide services to members after June 30, 2025.
- TrueCare will begin providing services to members starting July 1, 2025
Credentialed with a Delegated Credentialing Agency
If you credentialed through a delegated credentialing agency contracted with DOM and provided the agency name during your enrollment, you must follow the instructions outlined in the March 3, 2025 Late Breaking News article. Please see below for additional steps.
Joining the TrueCare Network
TrueCare is a Mississippi-based, non-profit, provider-sponsored health plan. It was established through a coalition of hospitals and health systems across the state and is supported by CareSource’s national expertise in quality and operational excellence. TrueCare offers locally based provider services with dedicated provider engagement representatives and customer support.
How to Begin the Contracting Process with TrueCare
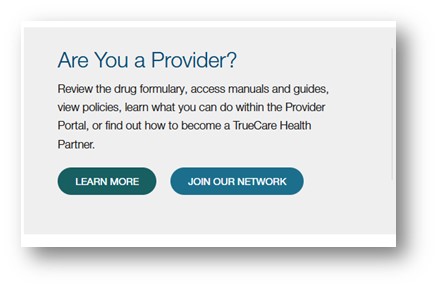
TrueCare offers two ways to begin the contracting process: online and offline.
Online Enrollment:
1. Visit the TrueCare website at MSTrueCare.com.
2. Click on “Join Our Provider Network.”
3. Locate the blue box and click “Start a Contract.”
4. Under Request Type, select New Contract.
5. Under Product Type, choose MS Medicaid – TrueCare.
6. Complete the Submitter Information and Contract Signatory Information sections.
7. Add your providers/locations.
8. Attach all required documentation.
9. Click Submit.
10. You will receive an auto-generated confirmation email upon submission.
Offline Enrollment:
1. To request a contract by email, please contact:
- Shelia Reed at Shelia.Reed@caresource.com
- Trisha Southerland at Trisha.Southerland@caresource.com
2. A contract will be sent to you for completion and return.
For more information, visit MSTrueCare.com.
Interested in Expanding Services to MSCAN and MSCHIP Members?
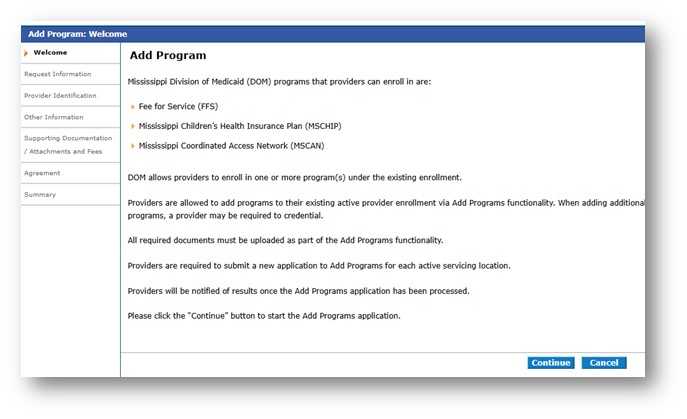
If you currently only provide services to fee-for-service members and wish to begin serving MSCAN and/or MSCHIP members, you can log into the MESA Provider Portal and follow the instructions to Add a Program. Please refer to the Add Program Job Aid for guidance. You must be credentialed through the Division of Medicaid before you can contract/enroll with any of the CCOs.
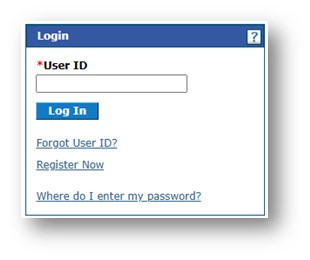
1. Login to the MESA Provider Portal.
2. Click the Add Program link to begin.
3. Provide the requested information and submit your details. For further guidance on the next steps following Medicaid approval, please refer to the specific credentialing type.
Interested in Serving Mississippi Medicaid Members?
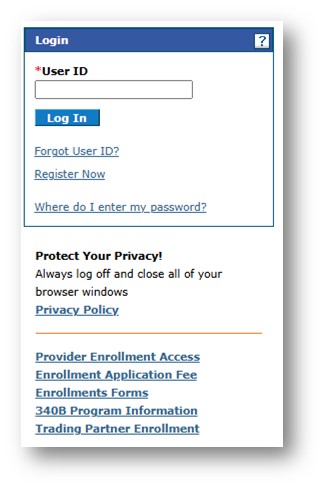
If you are not currently providing services to Mississippi Medicaid members but are interested in doing so, you may begin the enrollment process by following these steps:
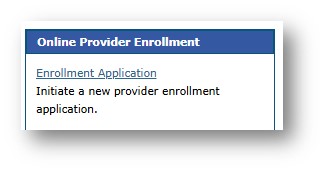
1. Navigate to the MESA Portal Home Page and select Provider Enrollment Access.
2. Choose Enrollment Application.
3. Complete all required fields and submit your application.
4. Promptly respond to any requests for additional information. Please note that failure to respond within 60 days will result in application denial.
5. Once your enrollment is approved, you may begin serving Fee-for-Service members immediately (if selected during the application process).
6. To serve members in Coordinated Care Organizations (CCOs), you must separately enroll and/or contract with each CCO you wish to join after completing Medicaid enrollment (if selected during the application process).
Find more Late Breaking News at: https://medicaid.ms.gov/late-breaking-news/.