Complete Your Renewal Online! – Click Here
Five Ways to Return Renewal Form – Click Here
PHE Unwinding Reports – Click Here
Stay Covered! Communications Toolkit – Click Here
Stay Covered! FAQs – Click Here
Update Your Contact Information Online
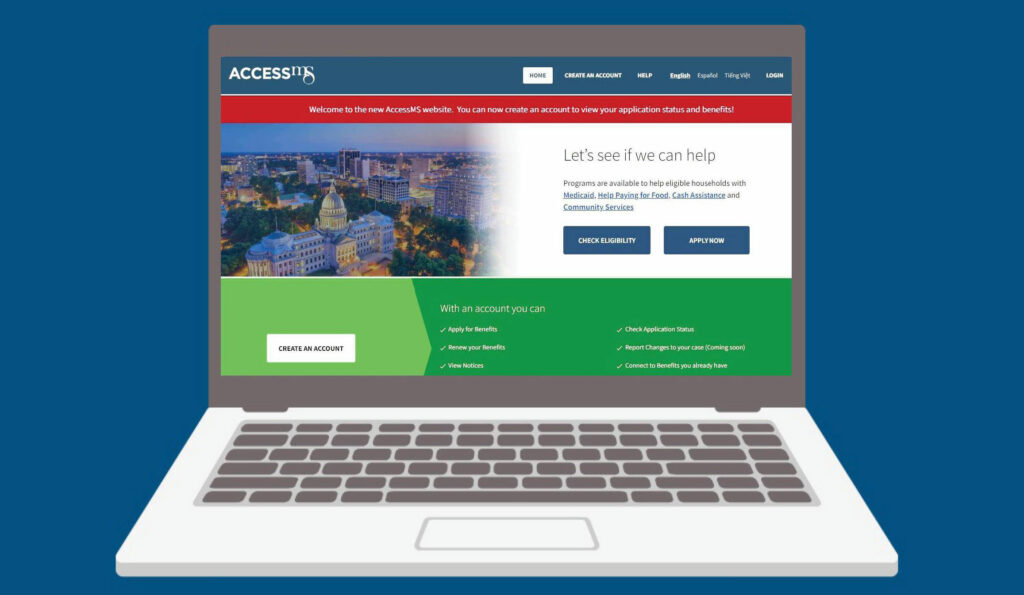
The Mississippi Division of Medicaid offers an option to update your contact information and complete your renewal online at Access.ms.gov. For instructions on how to complete your renewal online, click here.
For Medicaid Members
Resuming Routine Medicaid Eligibility Operations
In January 2020, the U.S. Department of Health and Human Services (HHS) declared a public health emergency (PHE) in response to the outbreak of COVID-19.
In March 2020, Congress passed the Families First Coronavirus Response Act (FFCRA) to help states respond to the COVID-19 pandemic . Under the FFCRA, the federal government provided states with a 6.2 percentage point increase in Federal Medical Assistance Percentage (FMAP). In exchange, states were prohibited in most circumstances from disenrolling members from Medicaid, even if they were found to be ineligible. This was to ensure members did not lose vital healthcare coverage during the pandemic.
. Under the FFCRA, the federal government provided states with a 6.2 percentage point increase in Federal Medical Assistance Percentage (FMAP). In exchange, states were prohibited in most circumstances from disenrolling members from Medicaid, even if they were found to be ineligible. This was to ensure members did not lose vital healthcare coverage during the pandemic.
In December 2022, Congress passed the Consolidated Appropriations Act (CAA). Per the CAA, the continuous coverage condition that prohibited states from disenrolling members from Medicaid will expire on March 31, 2023.
This means that states will resume routine eligibility operations, and the Mississippi Division of Medicaid (DOM) will begin re-qualifying all Medicaid members this spring.
It is very important for Medicaid members to update their contact information by clicking this link or calling DOM at 1-800-421-2408 or 601-359-6050.
You can also update your contact information online at www.medicaid.ms.gov/update-contact-info/.
When it is time for your requalification to take place, we will first try to renew your benefits by looking at electronic verification sources. If we are able to approve you using this method, there is nothing you will need to do. If we are not able to approve you this way, you will be mailed a renewal form and have 30 days to fill it out and return it back to us. That is why we need to have your most current mailing address and contact information.
If you currently have coverage, please do not submit a new application. Wait until you receive your renewal form and return it.
For Providers and Advocacy Groups
Planning for the end of the COVID-19 Continuous Coverage Requirement
The Mississippi Division of Medicaid will take 12 months to initiate renewals and 14 months to complete renewals for each of the approximately 880,000 Mississippians currently enrolled.
It’s essential that members update their contact information so they receive and return renewal packets to make sure they keep their Medicaid and CHIP coverage if they are still eligible.
An updated communications toolkit to provide information and guidance for anyone who interacts with Medicaid members will be released in the coming weeks.

Sign up to be a “Coverage Champion” and help us share important information and resources with Medicaid members.
How you can help: Coverage Champions
We need your partnership to ensure eligible members can keep their health coverage and those who no longer qualify know where they can go for affordable coverage resources. Sign up to be a Coverage Champion and help us share important information and resources, including the Stay Covered Flyer.
Use and share the materials in our toolkits to:
- Ask members to update their contact information so we can reach them.
- Educate yourselves on the renewal process so you can effectively help members.
- Inform members when they need to take action to keep coverage. Please do not tell members to complete a new application if they already have coverage (unless they are adding someone to their household or wanting to change their category of eligibility). This will bog down the system and may result in the member losing coverage if they are no longer eligible earlier than they otherwise would.